When is More Frequent Hemodialysis Beneficial?
In 2017, Medicare Administrative Contractors (MACs) began to promulgate draft local coverage determinations that include restrictive language regarding Medicare reimbursement for additional hemodialysis sessions. An important element of the draft determinations is medical justification, or the clinical conditions that constitute evidence-based rationale for the prescription of more frequent hemodialysis.
Suri and Kliger, who were both investigators in the Frequent Hemodialysis Network (FHN) trial, posed and answered this timely question in a thoughtful narrative review that appears in the July/August issue of Seminars in Dialysis.
Learn MoreCardiac Arrhythmia: An Ominous Side Effect of Thrice-weekly Hemodialysis?
Many studies represent incremental gains in our understanding of human pathophysiology. Some studies, especially large randomized clinical trials, can singlehandedly change the standard of care. Other studies, at the most unexpected times, flash a signal that raises the question of whether the widely accepted standard of care is simply inadequate.
In the April 2018 issue of Kidney International, Prabir Roy-Chaudhury and colleagues published one such study. These investigators reported data from a prospective, multicenter study, the Monitoring in Dialysis (MiD) Study, which was conducted in both the United States and India and aimed to estimate the proportion of thrice-weekly hemodialysis patients who experienced clinically significant arrhythmias during 6 months of follow-up.
Learn MoreACE Inhibitors or ARBs: Which to Prescribe?
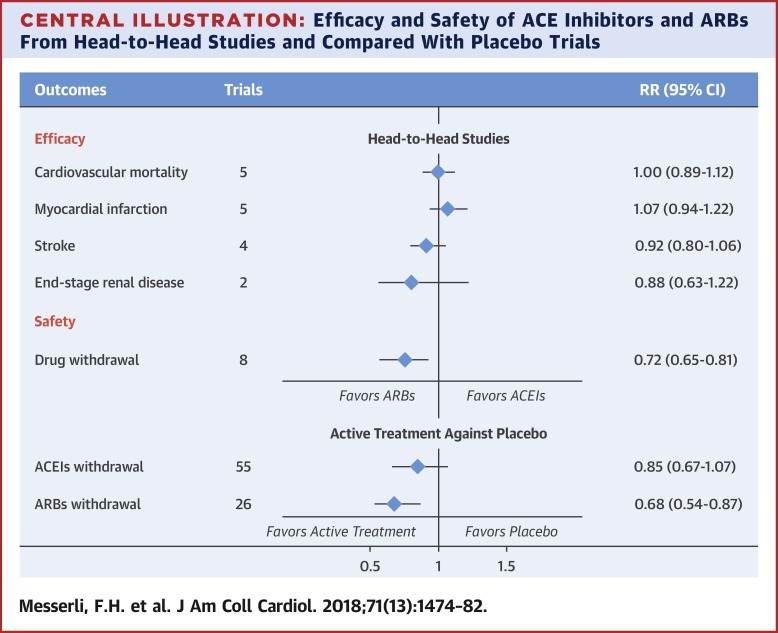
Many dialysis patients, including patients on frequent home hemodialysis, have been diagnosed with heart failure. In one large study, 31% of patients who initiated home hemodialysis already had heart failure.1 One of the cornerstones of pharmacologic therapy for heart failure is renin-angiotensin system blockade, which may be achieved with either angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs). In most clinical practice guidelines, ACE inhibitors are recommended as first-line therapy, while ARBs are recommended as a second option for patients who cannot tolerate an ACE inhibitor, typically because of a dry, persistent cough and atypically because of angioedema.
Learn MoreStandardized Kt/V on Home Hemodialysis: Does It Matter?
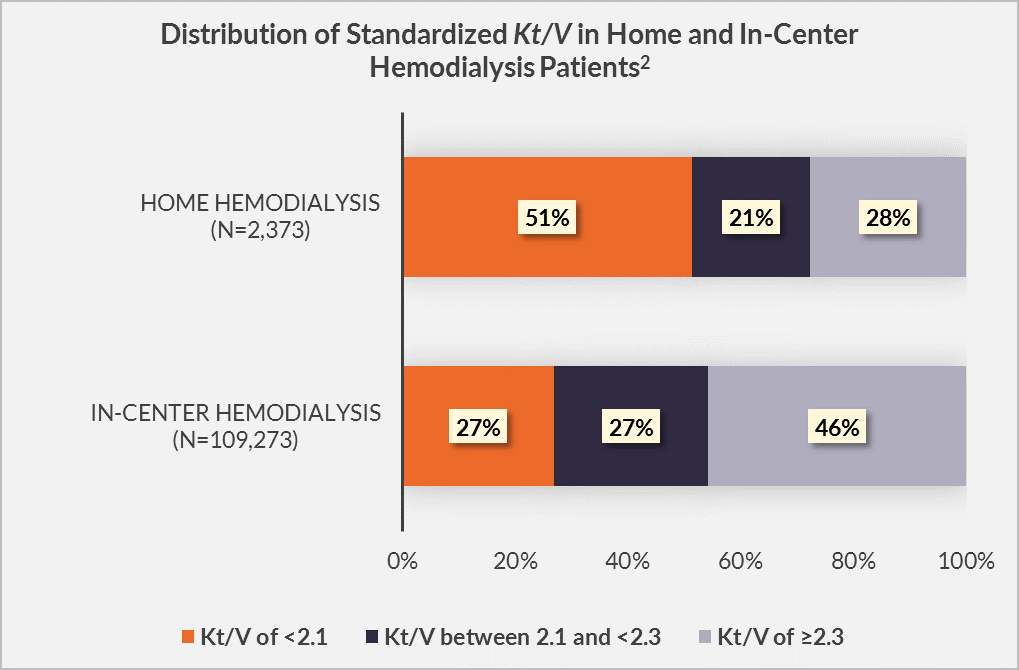
Hemodialysis adequacy has historically been assessed through the lens of Kt/V. Standardized Kt/V is a metric that specifically permits comparisons of urea clearance among heterogeneous hemodialysis schedules. Current clinical practice guidelines from the Kidney Disease Outcomes Quality Initiative (KDOQI) suggest a target standardized Kt/V of 2.3, and a minimal standardized Kt/V of 2.1.1 In principle, these targets are applicable to both in-center hemodialysis and home hemodialysis alike.
Learn MoreHypertension in Dialysis Patients
The link between hypertension, left ventricular hypertrophy, heart failure, and sudden death is clear. In the dialysis population, persistent hypertension is observed in the majority of patients, making it a fundamental and unmet challenge. Accumulating evidence shows that ambulatory blood pressure is a better predictor of survival than in-unit blood pressure—and, importantly, that ambulatory blood pressure is linearly associated with risk of cardiovascular events.1,2
As clinicians, how should we respond to this challenge?
Learn MoreInternational Guidelines for Increased Hemodialysis Time and Frequency
During the past 10 years, there has been a proliferation of research about intensive hemodialysis, including both longer and more frequent hemodialysis sessions. The accumulation of data from studies has led to the development of clinical practice guidelines about hemodialysis time and frequency, with a focus on identifying indications for increasing time and frequency.
In the United States, Medicare requires medical justification for reimbursement of additional hemodialysis sessions (i.e., treatment beyond 3 sessions per week). Clinical practice guidelines not only from the United States, but also from Japan, the United Kingdom, Europe, and Canada together encourage physicians to consider applications of longer and more frequent hemodialysis sessions in patients with cardiovascular complications, including left ventricular hypertrophy and uncontrolled hypertension; hemodynamic instability during dialysis, possibly due to excessive ultrafiltration intensity; hyperphosphatemia; and malnutrition.
Learn More