Transitioning from Peritoneal Dialysis to Hemodialysis
During the past decade, the use of peritoneal dialysis (PD) in the United States has grown substantially.1

In 2009, 7.5% of dialysis patients were treated with PD; by 2016, the statistic had increased to 10.0%.1 And according to the United States Renal Data System (USRDS), 10.5% of dialysis patients with new Medical Evidence Report (“2728”) submissions in 2017 were treated with PD.2 In addressing the goal of dialyzing more patients at home, this is a genuine accomplishment.
Although PD is a great modality for many patients, clinical complications such as catheter malfunctions, peritonitis, and ultrafiltration failure do occur, and lead some patients to transition from PD to hemodialysis (HD).3,4 According to data presented at ASN Kidney Week 2018, close to one in six patients who started on PD in 2015 had switched to HD within one year of initiation.5 Interestingly, between 2010 and 2015, the rate of conversion from PD to HD during the first year of PD was very stable.
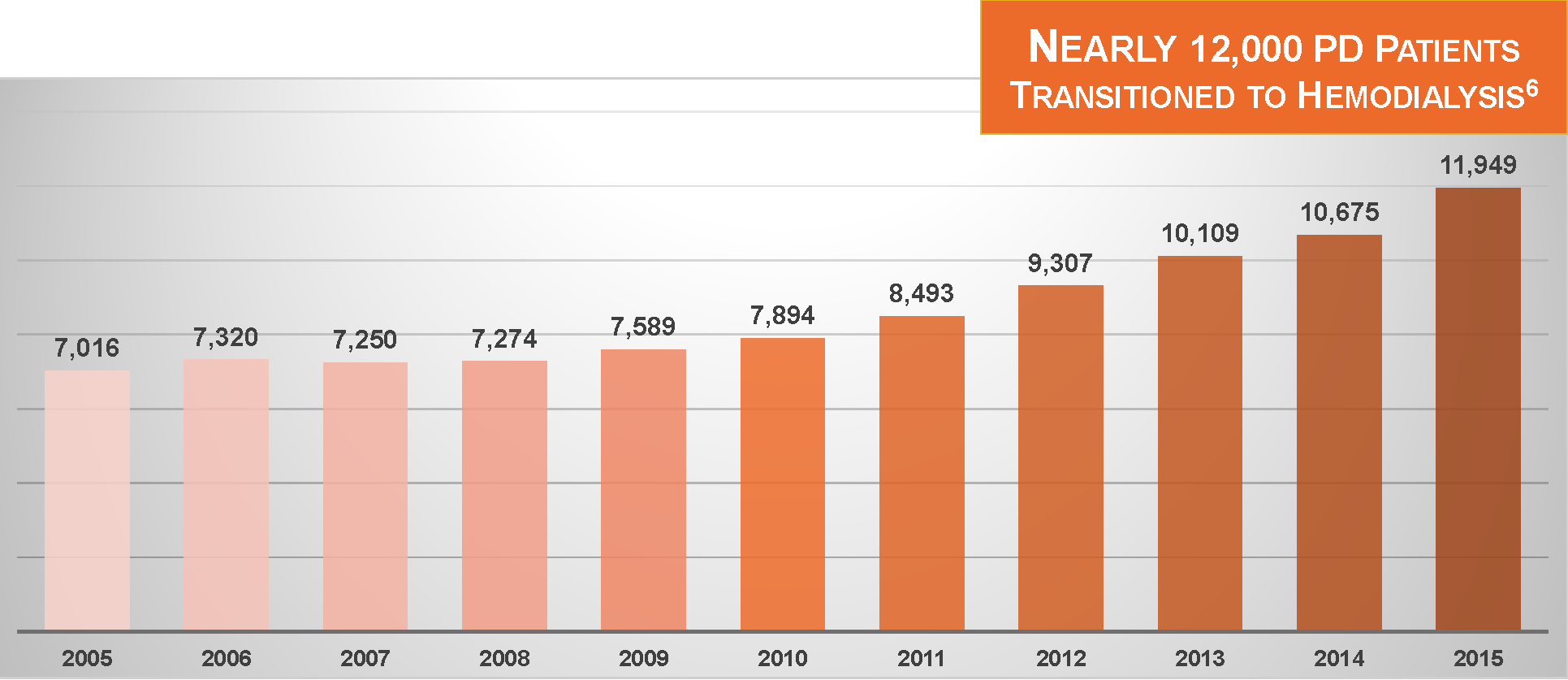
With a growing share of incident dialysis patients treated with PD, and a stable rate of conversion from PD to HD, at least during the first year of PD, the net effect is that the number of patients switching from PD to HD is steadily increasing. During 2015, almost 12,000 patients switched from PD to HD.6
Where do these patients go?
With few exceptions, they move into dialysis facilities, receiving in-center HD for 3 sessions per week and 3.0–4.5 hours per session. This is ironic, given that these are patients who expressed an interest in home dialysis at the beginning of their journeys with kidney failure. Shouldn’t it be possible to move patients from PD to HD, but allow them to continue dialyzing at home? From a psychosocial perspective alone, moving from PD to home hemodialysis (HHD) seems a natural choice.
In the current issue of Peritoneal Dialysis International, Sheru Kansal, Eric Weinhandl, and I analyzed USRDS data, assessing the incidence of and outcomes following conversion from PD to HHD, and comparing patients who switched from PD to HHD with patients who switched from PD to in-center HD.7
Several observations are noteworthy.
Transitions from PD to HHD are rare
We looked at U.S. patients initiating HHD with NxStage equipment between 2006 and 2012 and assessed their treatment history, as recorded in USRDS data, in the months preceding HHD initiation. We identified a total of 521 patients who switched from PD to HHD, despite permitting time on in-center HD between stints of PD and HHD. This amounts to roughly 75 patients per year in all the United States—a small number, but even smaller in context: during those same seven years, almost 33,000 (approximately 4,700 per year) patients switched from PD to in-center HD (and satisfied our inclusion criteria).
The bottom line is that a little more than 1% of patients who switch from PD to HD continue to dialyze at home; as an aside, the corresponding statistic in Australia and New Zealand is only slightly greater.8 Setting aside any claims about clinical implications of HHD and increased treatment frequency, this observation demonstrates a great opportunity to grow home dialysis in the United States.
Transitions from PD to In-center HD are common and costly
Among the 33,000 patients who switched from PD to in-center HD, the short-term rate of hospital admissions was exceptionally high. Keep in mind that we required that these patients remained alive for at least 2 months after the last day of PD, thereby eliminating the sickest patients who were hospitalized at the time of modality conversion and who died after only a few weeks of in-center HD.
Nonetheless, during the 6-month entry period—which comprised roughly 3–4 months of PD and 2–3 subsequent months of in-center HD—the mean number of hospitalized days in the subset of patients with Medicare fee-for-service coverage was 18.5, or the equivalent of 37 hospitalized days per year.
In 2012, the mean number of hospitalized days among all dialysis patients with Medicare fee-for-service coverage was 12.2.
Moving from PD to in-center HD was thus associated with a roughly threefold increase in hospitalizations—not good for patients, and not good for cost containment.
Imagine the toll that these hospitalizations take on actual expenditures in an ESRD Seamless Care Organization (ESCO).
Could transitioning from PD to HHD improve survival?
HHD appears to offer a path to better outcomes during and after the transition from PD to HD. In particular, we observed that:
- On average, patients who switched from PD to HHD were hospitalized only 9.1 days during the 6-month entry period.
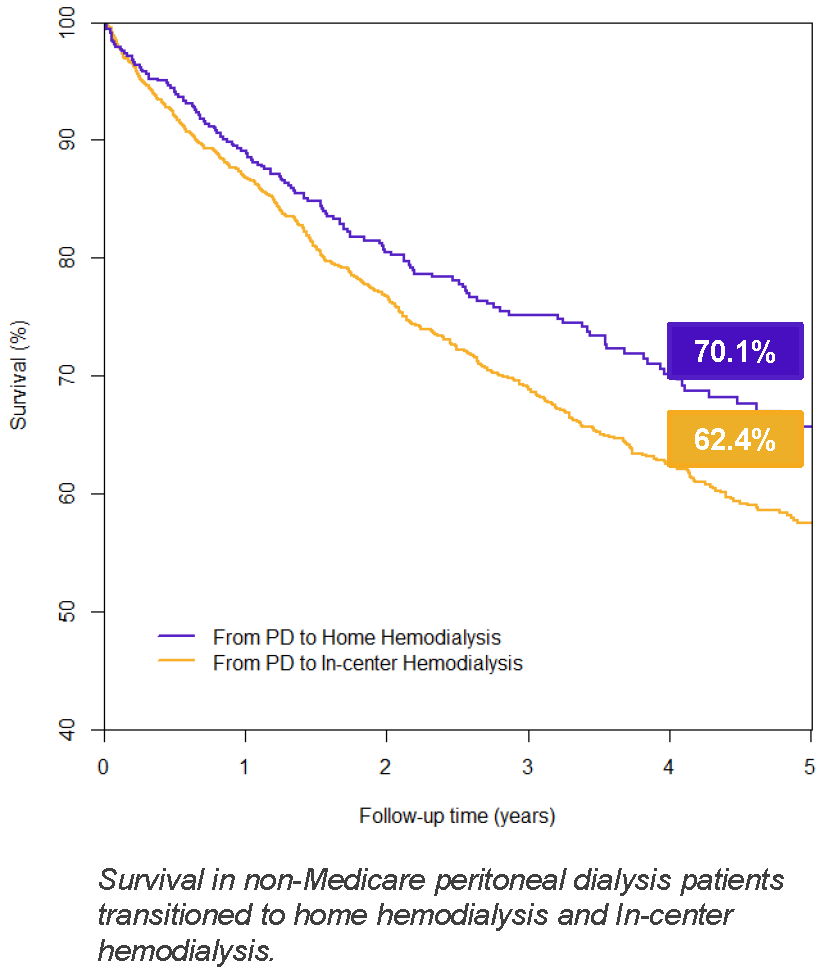
- After the transition to HHD, and relative to matched patients on in-center HD, patients on HHD exhibited significantly improved survival.
Could transitioning from PD to HHD increase transplantation incidence?
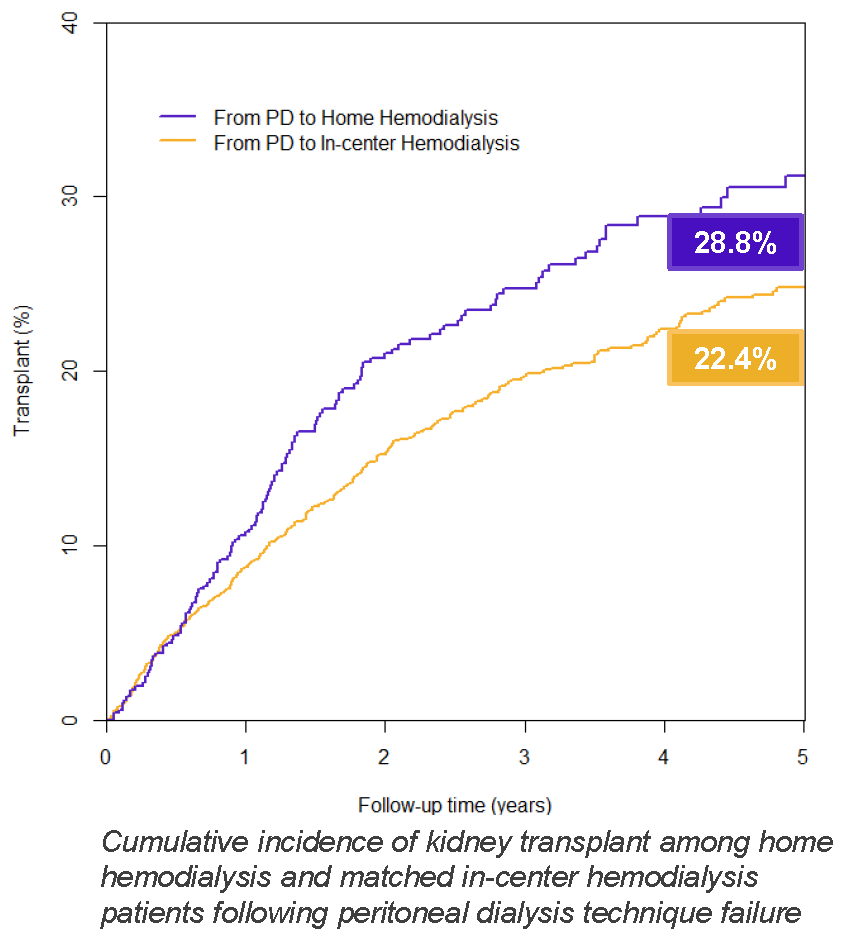
After the transition to HHD, patients exhibited significantly higher incidence of kidney transplant, relative to matched patients on in-center HD. The likelihood of transplant was 36% higher with HHD versus in-center HD.
This is an observational study, and any comparisons between HHD and in-center HD are subject to criticism. Not up for debate, however, is that a growing number of patients are moving from PD to HD each year, and that hospitalization is very common during the transition between modalities.
Could we do better?
At ASN Kidney Week 2018, an international group of researchers showed that the rate of death spikes after conversion from PD to HD in multiple regions of the world: Australia and New Zealand, Canada, the European Union, and the United States.9
HHD offers an opportunity for PD patients to continue dialyzing at home after PD becomes unviable, and also allows patients to dialyze more frequently. Increased treatment frequency may be especially important for patients who experience gradually deteriorating cardiac status during the final months on PD, as suggested by increased weight (due to volume expansion), rising blood pressure, and worsening left ventricular hypertrophy.
Ultimately, we are not the first party to suggest that transitioning from PD to HHD is a core component of an integrated home dialysis system.10
Take home message
Our study simply indicates that encouraging the transition from PD to HHD is an evidence-based approach. We have 12,000 (or more) chances each year to make this transition happen.6
Available Downloads
Potential Risks
Not everyone will experience the reported benefits of home and more frequent hemodialysis. All forms of hemodialysis involve some risks. When vascular access is exposed to more frequent use, infection of the site, and other access related complications may also be potential risks.
Certain risks associated with hemodialysis treatment are increased when performing solo home hemodialysis because no one is present to help the patient respond to health emergencies.
Certain risks associated with hemodialysis treatment are increased when performing nocturnal therapy due to the length of treatment time and because the patient and care partner are sleeping.
