Preparing for the future
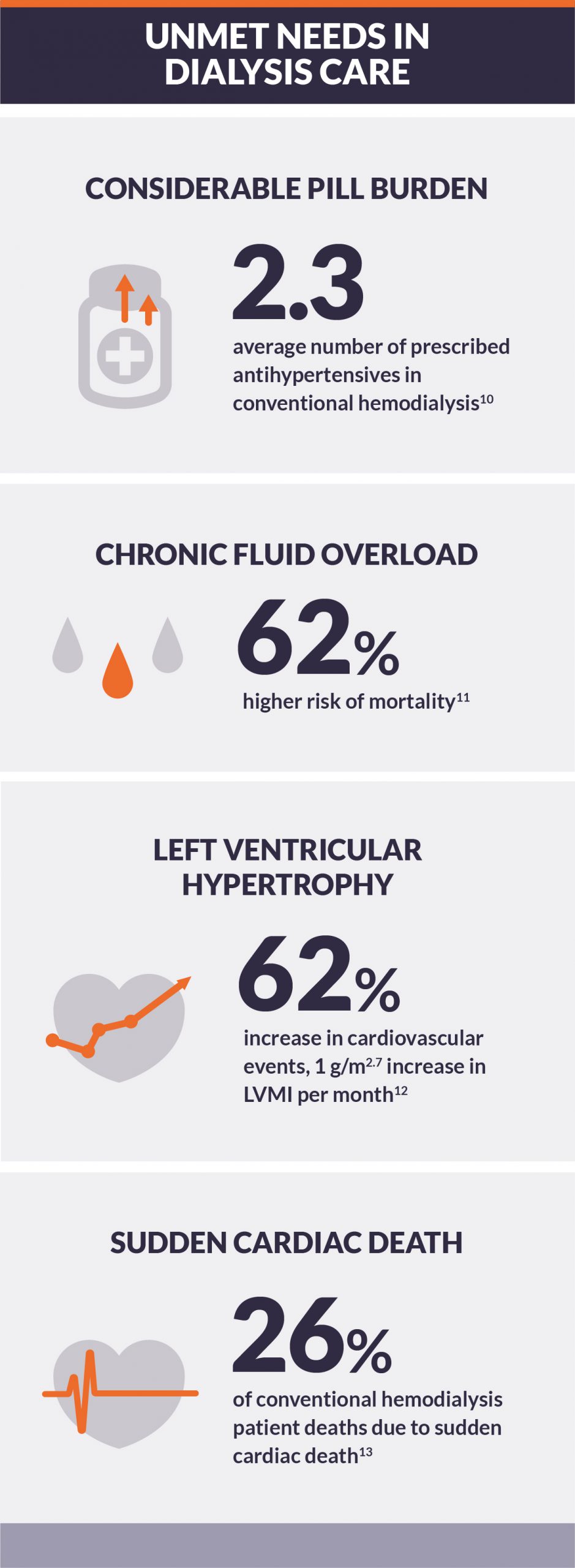
Dialysis populations around the world are rising.1,2 Although recent growth is almost completely attributable to improving survival, mortality rates remain much higher than in age-matched U.S. residents, and conventional, thrice-weekly hemodialysis may not adequately address:
High risk of cardiovascular morbidity and mortality3,4High pill burden5Diminished quality of life6,7Limited tolerability of conventional hemodialysis treatment8,9
To improve the quality of patients’ lives, intensive dialysis should be considered to address the fundamental complications that limit the long-term efficacy of conventional hemodialysis.
Learn MoreThe evidence is clear: intensive hemodialysis reduces left ventricular hypertrophy and may reduce risk of cardiovascular complications
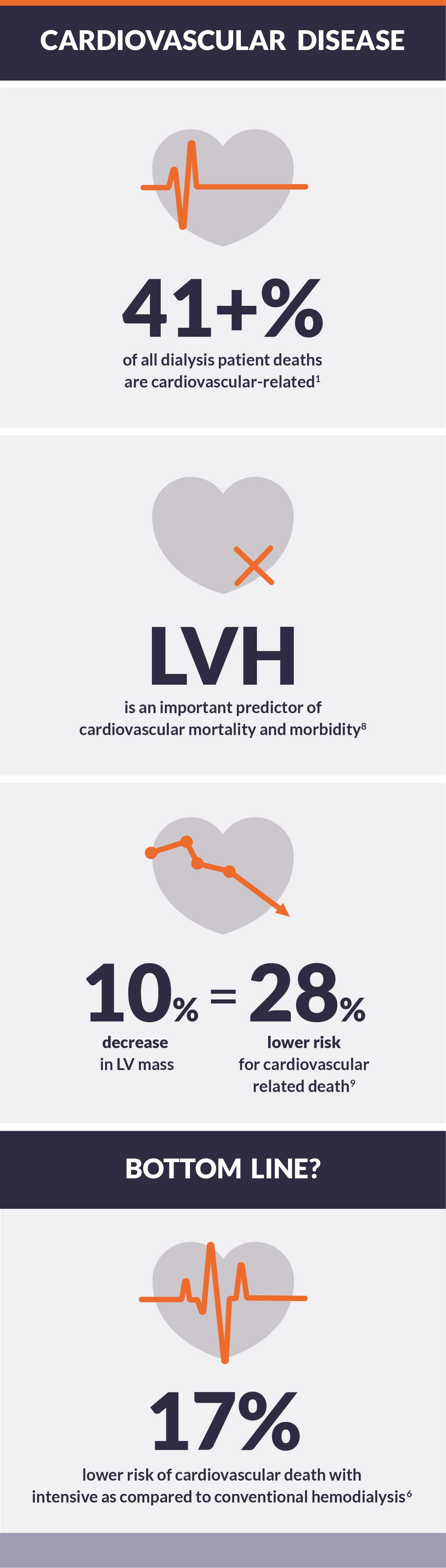
Cardiovascular death is significantly more likely in dialysis patients than in age-matched, community-dwelling adults in the U.S., despite dramatic increase in the use of cardioprotective medications.1 New strategies are clearly needed to improve cardiovascular health in dialysis patients. Because left ventricular hypertrophy (LVH) is an important predictor of cardiovascular mortality and morbidity, strategies to reduce LVH are likely to reduce cardiovascular disease risk in patients.2
Intensive dialysis reduces LVH
Multiple randomized clinical trials show that intensive hemodialysis reduces left ventricular mass:
In the Frequent Hemodialysis Network trials, short daily and nocturnal schedules, each for six sessions per week, reduced left ventricular mass by 10% and 8%, respectively, relative to three sessions per week.
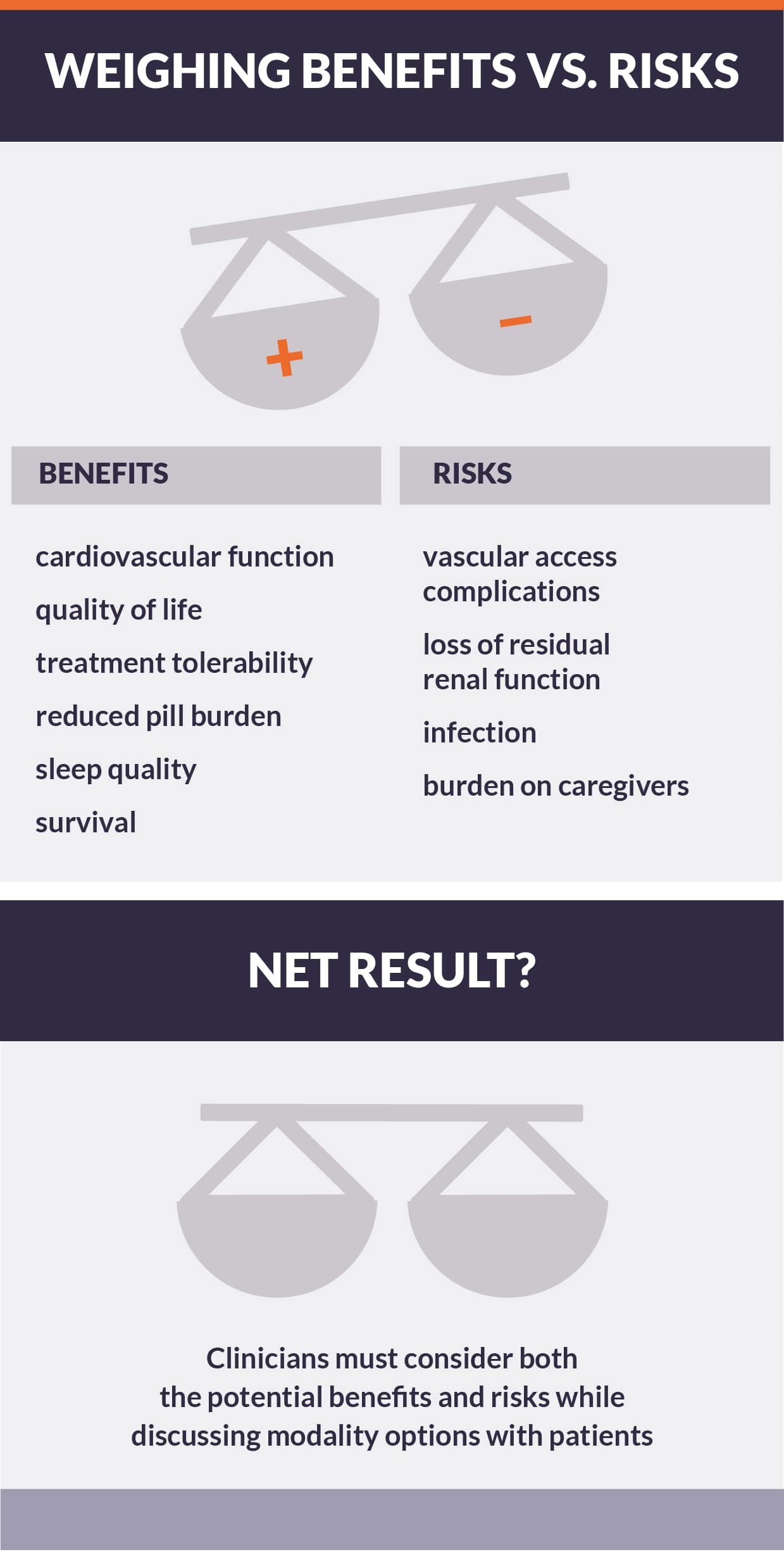
Learn MoreA question of balance: Benefits vs. risks of intensive hemodialysis
Although intensive hemodialysis may address important clinical problems, increasing treatment may introduce risks pertaining to six domains: vascular access complications, infection, mortality, loss of residual renal function, solute balance, and patient and care partner burden.
Trials have shown increased access complications and infection
In the Frequent Hemodialysis Network (FHN) trials, short daily and nocturnal schedules increased incidence of access complications, most commonly due to infection, although incidence of access loss was not statistically elevated. 1Observational studies regarding vascular access complications are mixed.
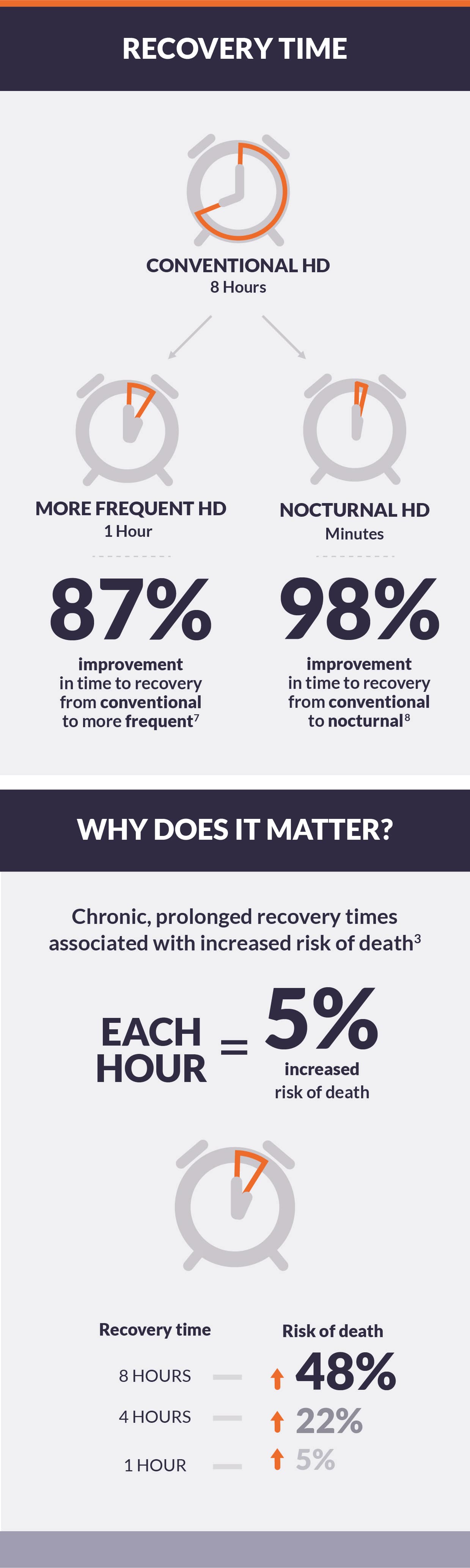
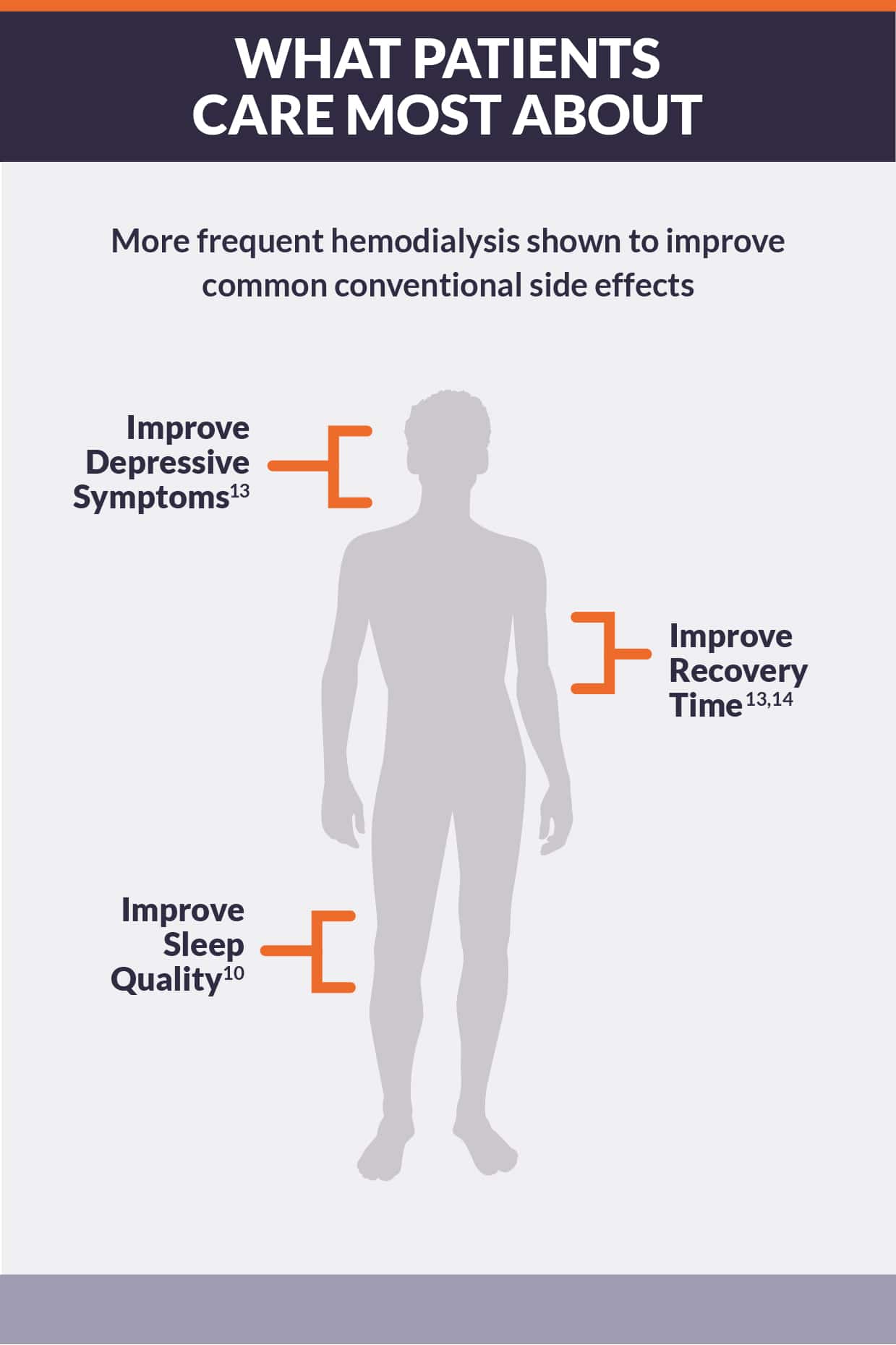
Learn MoreIntensive hemodialysis reduced post-treatment fatigue and recovery time
Hemodialysis can be difficult to tolerate. Common complications are intradialytic hypotension and long recovery time after treatment.1 Intradialytic hypotension may be caused by aggressive ultrafiltration in response to interdialytic weight gain, related to myocardial stunning and cardiac arrhythmias, and is associated with increased risk of death.2 Long recovery times may impair physical and mental function and decrease qualify of life.3 Patients and caregivers rank fatigue more highly than any other problem, including life expectancy.
Learn MoreIntensive hemodialysis has improved physical and mental health-related quality of life
Dialysis patients commonly present limitations in both physical and mental health-related quality of life (HRQOL), with an especially high prevalence of depression.1,2 Poor HRQOL may be partially due to inadequate dialysis, resulting in physical symptoms.3 Diminished health-related quality of life is associated with increased risks of morbidity and mortality.4
Studies show intensive hemodialysis may positively impact HRQOL
In three randomized clinical trials comparing intensive and conventional hemodialysis, intensive hemodialysis increased physical and mental component summary scores from the 36-Item Short Form Health Survey (SF-36).
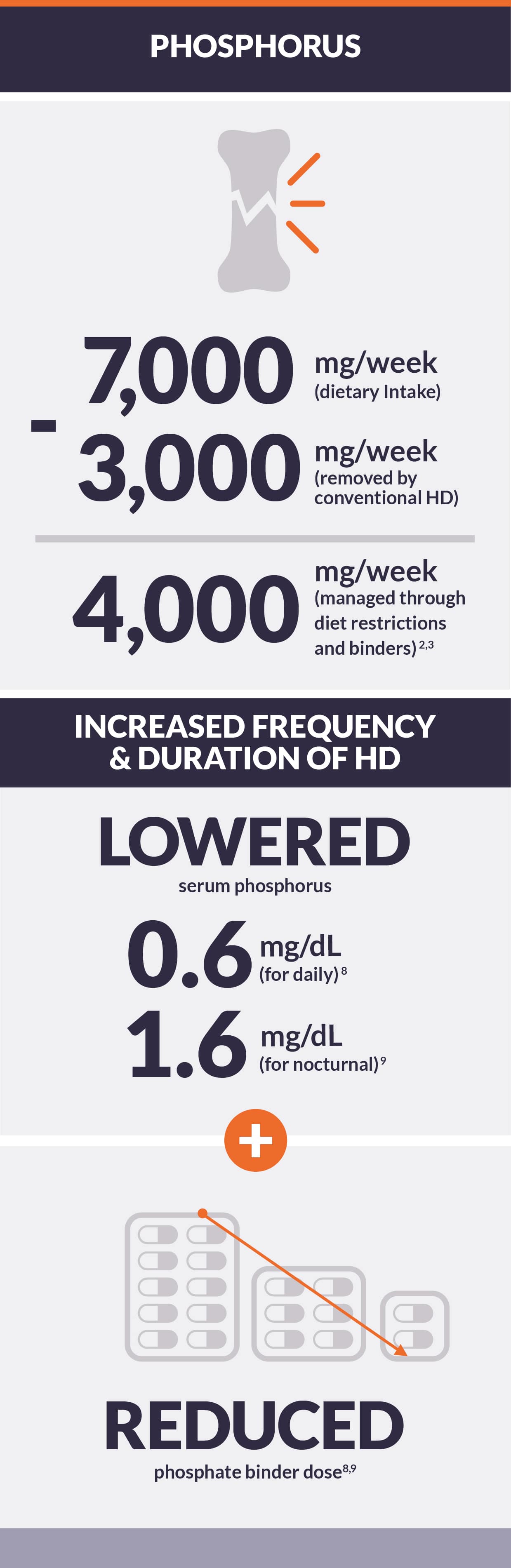
Learn MoreIntensive hemodialysis has reduced serum phosphorus and phosphate binder use
Mineral and bone disease is a common complication of kidney failure.1 There is a significant gap between phosphorus absorption and clearance in conventional hemodialysis.2,3 In 2015, over 36% of hemodialysis patients had serum phosphorus persistently above the target range.4 Hyperphosphatemia is associated with higher risk of cardiovascular mortality and morbidity, but treating hyperphosphatemia with phosphate binders is burdensome to both patients and payers.1,5,6,7
Trials show intensive hemodialysis reduced serum phosphorus and the need for phosphate binders
Multiple randomized clinical trials show that intensive hemodialysis reduced serum phosphorus:
In the Frequent Hemodialysis Network trials, short daily and nocturnal schedules, each for six sessions per week, reduced serum phosphorus by 0.6 and 1.6 mg/dL, respectively, relative to three sessions per week.
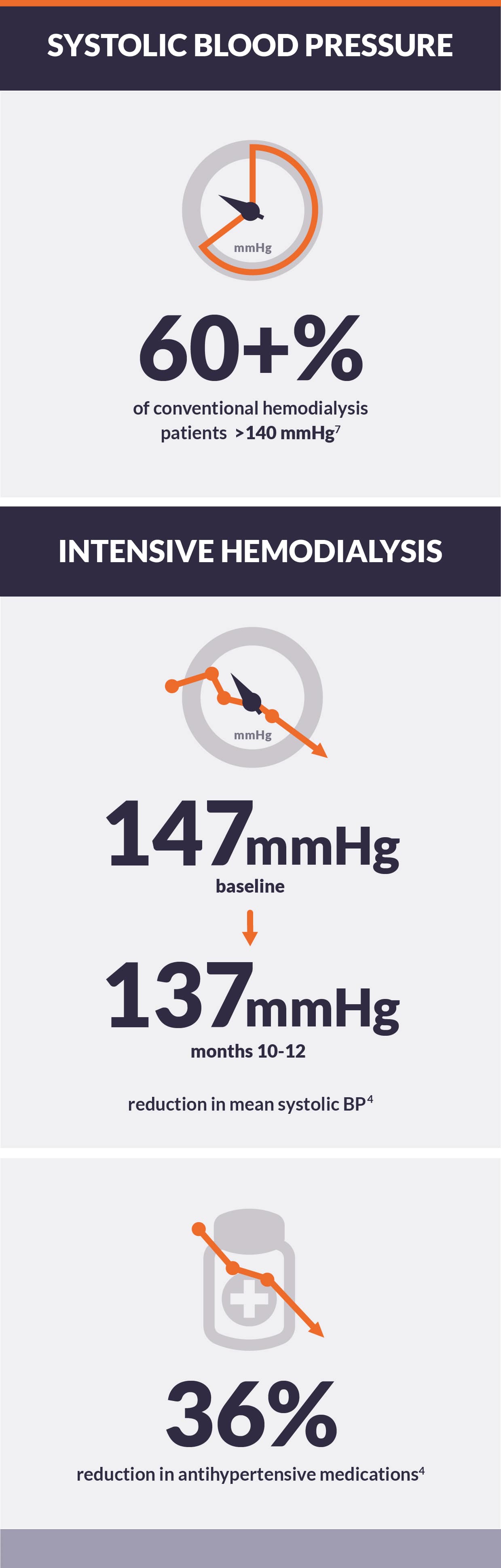
Learn MoreIntensive hemodialysis improves blood pressure control and reduces need for antihypertensive agents
Persistent hypertension is a vexing problem in the care of dialysis patients.1 Perennially, blood pressures over 140/90 are the second leading cause of kidney failure in the U.S.2 Antihypertensive medications are widely used and polypharmacy is common, but pharmacologic intervention is often unsuccessful at lowering blood pressure to normotensive levels.3
Trials have shown intensive hemodialysis reduces blood pressure
In the Daily Trial of the Frequent Hemodialysis Network, intensive hemodialysis reduced pre-dialysis systolic blood pressure (SBP) by 7.7 mmHg, relative to three sessions per week.
Learn More