Increasing transplantation incidence
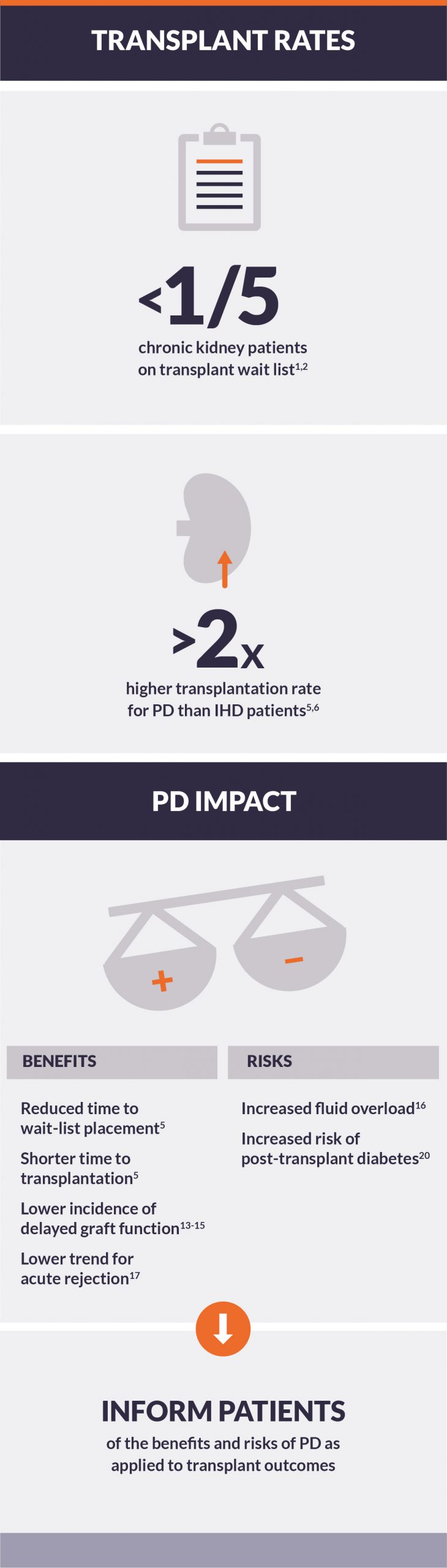
Of the more than 500,000 patients on chronic dialysis in the US, less than one-fifth are active on the kidney transplant waiting list —despite broad agreement on the economic and quality-of-life benefits to transplant.1-3 Several factors influence this, including graft availability, wait time, and post-transplant viability.
Wait-list placement time and transplantation incidence
Most incident ESRD patients are prescribed conventional hemodialysis (IHD) over peritoneal dialysis (PD) in the United States.1 This is despite findings that PD may be a better pre-transplant dialysis modality.4
- PD patients experienced a 32% reduction in wait time for placement on the transplant waiting list, an increased rate of being on the waiting list, and a shorter time to transplantation as compared to IHD patients.5
- Unadjusted transplant rates for incident PD patients has been reported as more than twofold higher than for HD patients.5,6
- In a study of 620,020 IHD and 64,406 PD patients, adjusted transplant rates in PD were 30% to 60% higher relative to IHD.7
Influence of social support and dialysis adherence
Social support scores have been shown to be higher in PD than IHD patients and associated with better patient-centered outcomes—including greater patient satisfaction and health-related quality of life, increased transplantation, and reduced hospitalization.8-11
- In a survey of 584 transplant providers, respondents were 1.68 times more likely to choose a profile of a transplant candidate who had social support, and 1.64 times more likely to choose one who always adheres to his/her medical regimen.12
- Nephrologists who offer explicit treatment recommendations and tailor discussions of suitable treatment options to patients were more influenced by adherence and quality of life than medical/surgical providers who were more influenced by candidates’ life expectancy with transplant.11
- Social support was the most influential factor for providers concerned with avoiding organ waste, while least influential for clinicians concerned with fairness (p<0.05).11
Delayed graft function and acute rejection
A few studies have shown lower incidence of delayed graft function after kidney transplantation in PD patients compared with IHD patients.13-15 Factors involved may include patient fluid status and residual kidney function at the time of transplantation.
- Pre-transplant PD use was associated with improved fluid status and a 36% lower risk of delayed graft function risk compared to pre-transplant IHD.16
- A recent study showed a 14% improvement in 5-year survival and a trend of lower acute rejection rate in use of PD compared to IHD before transplantation.17
Pre-transplant PD impact on weight, mortality risk, and post-transplant diabetes
Volume overload remains a greater problem for PD patients than for those on IHD.18 Body weight reduction post-transplant has been shown to be significantly higher with PD compared to IHD, indicating increased fluid overload in PD patients prior to transplantation.16
- Even with pre-transplant IHD support to improve volume status, PD patients still showed a 5% extracellular fluid volume excess before transplantation.16
- Despite difficulties in achieving dry weight, use of PD prior to transplantation had a 43% lower adjusted all-cause and 66% lower cardiovascular death compared to use of IHD.16
- Results of pre-transplant PD use and graph failure are mixed. Confounding by residual selection bias cannot be ruled out and merits further investigation.19
- In a recent study, pre-transplant PD has been associated with 17% lower unadjusted death-censored graft failure.19
- In contrast, in an analysis using a propensity score-matching algorithm in IHD vs. PD patients before transplantation, PD patients experienced similar graft loss.19
- Pre-transplantation use of PD has also been shown to significantly increase the risk of post-transplant diabetes mellitus development.20
Conclusion
Evidence indicates that pre-transplantation use of PD positively affects post-transplantation outcomes. Transplantation incidence, transplantation rate, and post-transplantation graft function have been shown to be better in patients who used PD pre-transplantation compared to IHD. However, fluid management during PD is crucial and transplant-provider bias could be an obstacle to transplant candidacy. Patients should be informed of the benefits and risks of PD as applied to transplant outcomes.