Peritoneal dialysis and residual kidney function
Many peritoneal dialysis (PD) patients initiate therapy with some residual kidney function (RKF). The importance of preserving this RKF and minimizing the potential for further kidney injury cannot be overstated.1,2,3 It is well established that end-stage kidney disease patients with substantial RKF live longer. Both glomerular filtration rate (GFR) and urine volume have been associated with improved survival in numerous studies.3
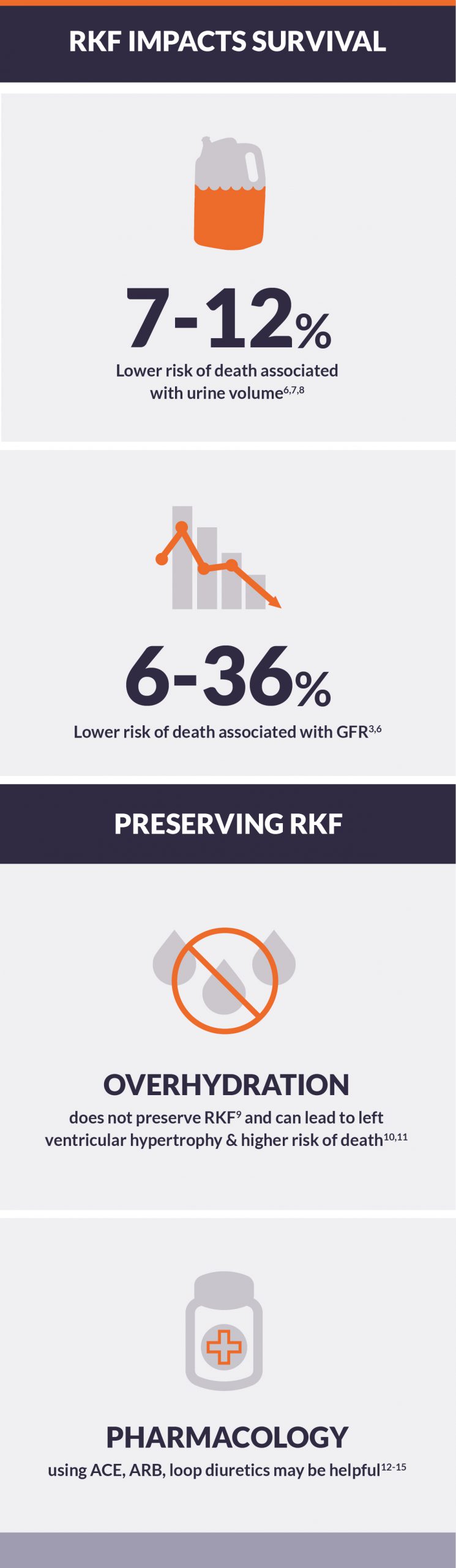
Preservation of RKF and survival
RKF in peritoneal dialysis patients appears to be more strongly associated with survival than peritoneal clearance.1
- In a large study that included 692 PD patients in Korea, each 100-mL increment in 24-hour urine volume was associated with 6% lower risk of death, following adjustment for demographic and clinical factors.4
- In a re-analysis of the CANUSA study, each 0.5-mL/min/1.73m2 increment in GFR was associated with 12% lower risk of death; each 250-mL increment in 24-hour urine volume was associated with a 36% lower risk of death.5
- In the NECOSAD study, which included patients with incident end-stage kidney disease who initiated PD, each 1-mL/min/1.73m2 increment in GFR was associated with 12% lower risk of death.6
- Data from Australia and New Zealand exhibit a similar pattern: each 1-mL/min/1.73m2 increment in GFR was associated with 7% lower adjusted risk of death.7
Importantly, PD is associated with better preservation of RKF than conventional hemodialysis (IHD).8
- In the NECOSAD study, the adjusted rate of decline in GFR over 12 months was 8.1% per month with PD and 10.7% per month with IHD.6
Overhydration does not preserve RKF
Despite the evidence in the literature to the contrary, a common belief in clinical practice has been that mild overhydration can preserve RKF in PD patients.
- Relative overhydration, as measured by bioelectrical impedance analysis, is not associated with preservation of RKF.9
- Overhydration is associated with left ventricular hypertrophy and higher risk of death, as shown in the Initiative for Patient Outcomes in Dialysis-Peritoneal Dialysis (IPOD-PD) study.10,11
Pharmacologic therapies can aid in preserving RKF
Recent guidelines state the preferential use angiotensin-converting enzyme (ACE) inhibitor or angiotensin-II receptor blocker (ARB) as the first-line antihypertensive agents for patients on PD.3 Small clinical trials suggest possible value of renin-angiotensin system inhibitors:12,13
- In a trial of 34 Japanese patients on continuous ambulatory PD, treatment with valsartan, an ARB, significantly slowed the decline of GFR.12
- In another trial of 60 Hong Kong patients on PD, treatment with ramipril, an ACE inhibitor, likewise slowed the decline of GFR.13
Large doses of loop diuretics (500-2000 mg/day) have been shown to increase urine volume; smaller doses may also be helpful:14
- A study of 61 patients on continuous ambulatory PD found that 250 mg/day of loop diuretics preserved urine volume after one year, although the treatment failed to slow decline of GFR.15
Certain pharmacologic therapies should be avoided in dialysis patients
- Aminoglycosides and non-steroidal anti-inflammatory drugs are often cited as being able to preserve RKF; however, observational studies have failed to substantiate associations of exposure with loss of RKF and prolonged use (>3 weeks) is associated with risk of ototoxicity.1,3
- Other potential nephrotoxic agents such as IV contrast should be used with caution.3
Conclusion
RKF, as measured by either GFR or urine volume, is an important predictor of positive clinical outcomes, including longer survival. Notably, PD is associated with better preservation of RKF than conventional hemodialysis. However, it is important that PD always aims for euvolemia, as relative overhydration on PD fails to preserve RKF (and may increase risk of death). If adjunctive therapies are required, ACE inhibitors, ARBs, and loop diuretics may be useful.