Kidney Care Choices Voluntary Payment Models
The current Medicare payment system encourages in-center hemodialysis as the default treatment for patients beginning dialysis. In 2019, 85% of those with incident end-stage kidney disease (ESKD) initiated in-center hemodialysis.1 Many Medicare ESKD beneficiaries suffer from poorer health outcomes, such as higher hospitalization and mortality rates, often the result of underlying disease complications and multiple co-morbidities.2 On January 1, 2022, the Centers for Medicare and Medicaid Services (CMS) launched the first performance year of a new voluntary payment model to help manage care for Medicare beneficiaries: Kidney Care Choices (KCC).
New Value-Based Care Incentives for Providers3
KCC incentivizes dialysis facilities, nephrologists, and/or other healthcare providers form ESKD-focused accountable care organizations to manage care for ESKD Medicare beneficiaries. The KCC models will be in effect for five years, allowing healthcare providers in them to take on accountability for the cost and quality of care for Medicare beneficiaries with chronic kidney disease (CKD) stages 4 and 5, and ESKD, to delay the onset of dialysis and to incentivize kidney transplantation.
Medicare Beneficiary Alignment and Value-Based Care Goals4
CMS assesses claims data and aligns patients based on outpatient encounters with nephrologists in the model. For CKD 4 and 5, CMS will align eligible beneficiaries with two encounters during a 12-month period. ESKD Medicare beneficiaries with be aligned if there are at least two monthly capitation payment (MCP) claims over a three-month period.
These parameters help to align Medicare beneficiaries to KCC participants in order to help health care providers reduce the cost and improve the quality of care.
Delaying the progression to ESKD
Previous guidelines suggested initiating dialysis prior to the appearance of uremic symptoms, or at an estimated glomerular filtration rate (eGFR) of ≤15 mL/min per 1.73 m2.5
Between 2000 and 2010, there was a significant increase in the percentage of patients initiating kidney replacement therapy with an eGFR ≥10 ml/min/1.73m2 from 23% to 43%.1 Since 2010, there has been a reversal in this trend.
In 2010, data published by the Initiating Dialysis Early and Late (IDEAL) study indicated that planned early initiation of dialysis in patients with stage 5 CKD was not associated with an improvement in survival or clinical outcomes.6
Presently, 48% of patients initiate dialysis with an eGFR of between 5–10 mL/min/1.73 m2, 28% initiate dialysis with a eGFR between 10– 5 mL/min/1.73 m2, and only 11% of patients initiate dialysis with an eGFR ≥15 mL/min/1.73m2.1
Encouraging optimal transitions to dialysis
Optimal ESKD starts are defined as the percentage of new adult ESKD patients during the KCC measurement period who experience a planned start of renal replacement therapy by receiving a preemptive kidney transplant, by initiating peritoneal dialysis, or by initiating hemodialysis via arteriovenous fistula or arteriovenous graft.7
Supporting patients through the transplant process
Not only does the KCC beneficiary alignment take into consideration where a beneficiary receives the majority of their kidney care, it also is grounded in a patient’s most valued source of transplant education: their nephrologist.
In a survey of patients—actively waitlisted for a kidney transplant, received a kidney transplant, had CKD, or were on dialysis—almost half (48%) cited their nephrologist as their primary source of information about transplant centers. Only a small percent of patients reported using the Scientific Registry for Transplant Recipients (9.7%).8
Keeping transplant beneficiaries healthy, post-transplant
When an aligned beneficiary receives a kidney transplant, they will remain aligned to the model participant for three years following a transplant in order to track transplantation outcomes.
KCC Model Designs
CMS Kidney Care First (KCF) uses adjusted capitated payments and limits eligible providers to nephrology practices and their nephrologists.
Comprehensive Kidney Care Contracting (CKCC) includes three options that use adjusted capitated payments and allow for a variety of providers through Kidney Contracting Entities (KCE) to take responsibility for patient costs and outcomes.
These model designs include five common elements:
- Timeline
The voluntary models began January 1, 2022, and will end December 31, 2026. - Required minimum Medicare beneficiary counts
| KCC Model | CKD 4-5 Patients | ESKD Patients |
|---|---|---|
| KCF | 400 | 200 |
| CKCC | 750 | 350 |
- Transplant bonus
Participants can receive up to a $15,000 bonus if kidney transplants remain functional for 1, 2, and 3 years. CMS pays transplant bonuses to the KCC participating practices or the CKCC Kidney Contracting Entities (KCE) quarterly following the 1-, 2- and 3-year anniversary of allograft function. - CKD quarterly capitation payment (CKD QCP)
Instead of receiving a payment for each outpatient service provided to the aligned stage 4 or 5 patient, this model makes a lump sum advanced payment on a quarterly basis to the KCF practice or to the KCE. These CKD 4 and 5 payments include, but are not limited to, office evaluation and management visits, established patient home visits, and advanced care planning. - Positively adjusted home dialysis payment
CMS will pay an additional $35 per home dialysis MCP claim on an annual basis to KCC participants in an effort to make those payments comparable to the payments received for seeing an in-center hemodialysis patient four or more times per month.
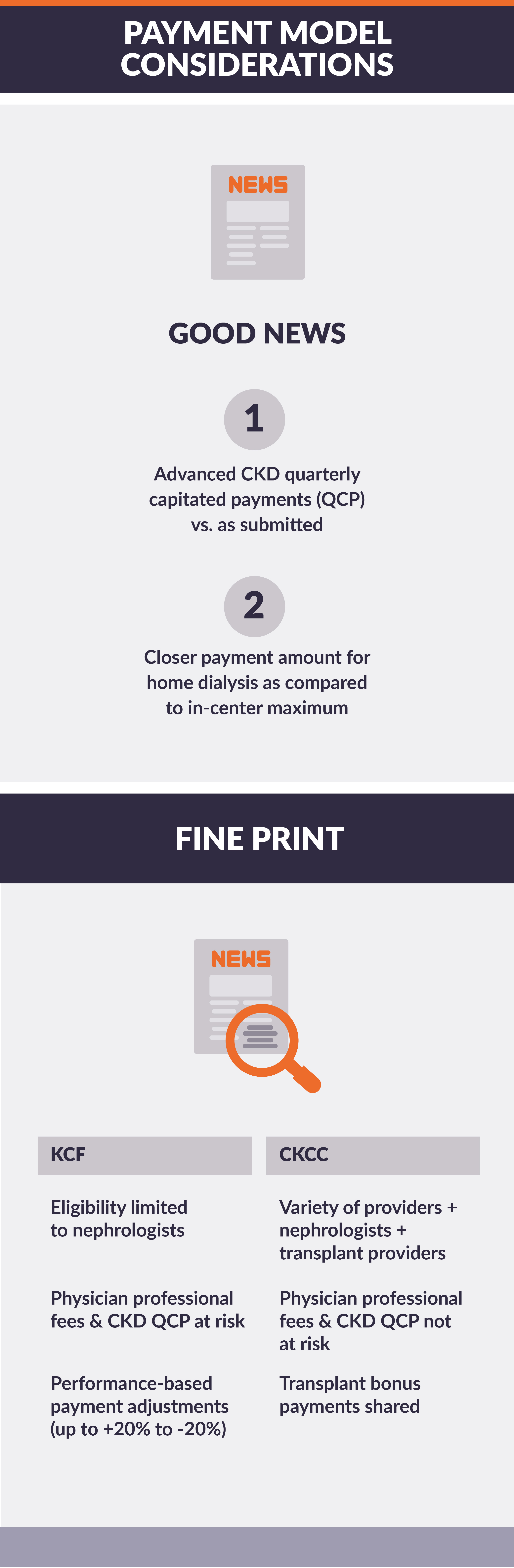
Pro or Con: CKCC or KCF?
Patient-centered improvement measures, such as gains in patient activation scores at 12 months (NQF #2483), depression remission or progress towards remission at 12 months (NQF #1885), and optimal dialysis starts (NQF#2594), are positive quality and utilization measures for both KCC models.
Both models, however, have tradeoffs. These tradeoffs are pervasive when deciding between participating in a total-cost-of-care model versus a performance-based fee-for-service model.
For participants in the CKCC model, although payments are not subject to a performance payment adjustment, the transplantation bonus must be split up as follows: 20% to the nephrologists, 20% to the transplant provider, and the balance divvied up as the KCE sees appropriate.
For participants in the KCF model, nephrologists and nephrology practices will receive adjusted fixed payments on a per-patient basis, with the payments adjusted based on quality health outcomes for the beneficiaries and utilization across the practice.
For the top 25% of KCF practices, the performance payment adjustment is up to +20%. In comparison, for practices that are below the 50th percentile for KCF practices and in the bottom quartile of all nephrology practices nationally, the performance adjustment is -20%. The -20% adjustment also applies to practices that fail to pass a minimum quality threshold referred to as the Quality Gateway. The payment adjustments are applied to the CKD QCP and all MCP Medicare claims.
Conclusion
KCC aims to be a patient-centered program by promoting patient activation and mental health. It includes multiple benefit enhancements as well as a focus on slowing the progression of CKD, with optimal transitions to kidney failure treatment modalities should kidney failure occur.9 The benefits enhancements target improved education, easy access, and coordinated care to reduce admissions and readmissions and decrease the cost of care.