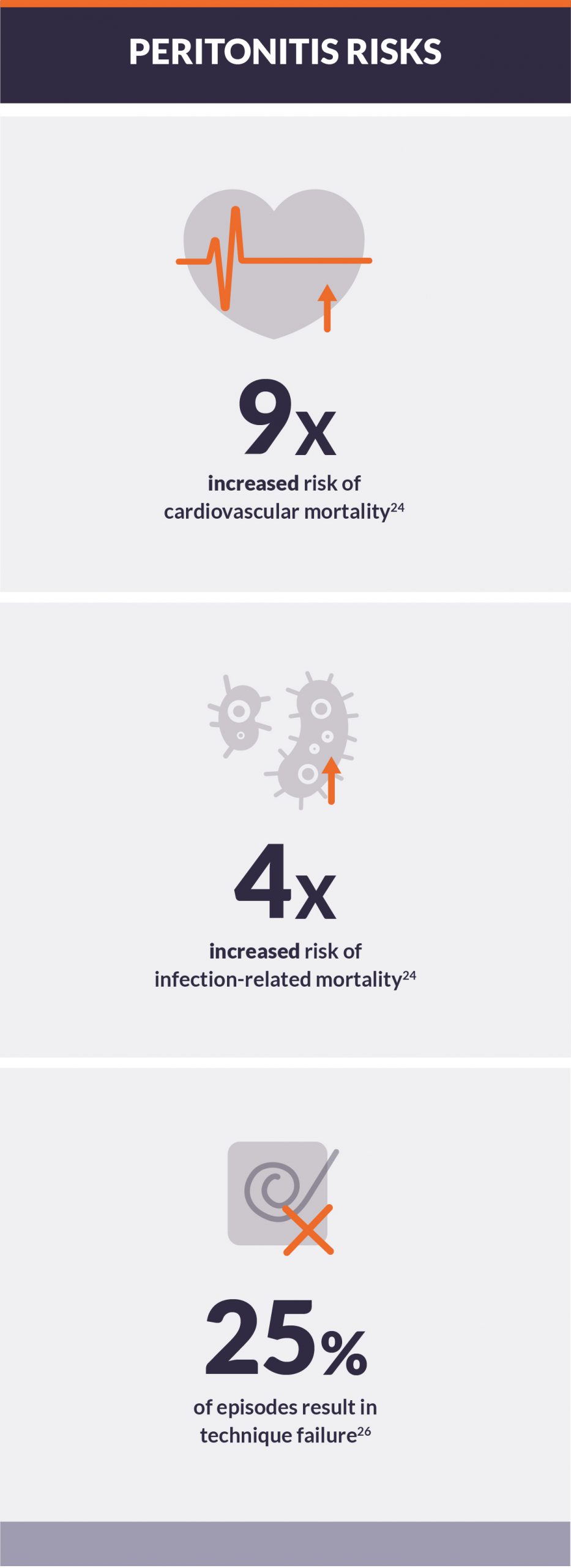
Peritonitis in peritoneal dialysis
Peritonitis is the most serious infectious complication associated with peritoneal dialysis (PD) therapy.1 Peritonitis rates have shown significant improvement over the years, with recent data reporting infection-related hospitalizations experienced by 16% of peritoneal dialysis patients.2 However, infection-related deaths accounted for 10% of PD patients versus 7% of conventional hemodialysis (IHD) patient deaths.3 Secondary complications of PD-related infections significantly compromise long-term use of the peritoneal membrane, patient well-being, and longevity.
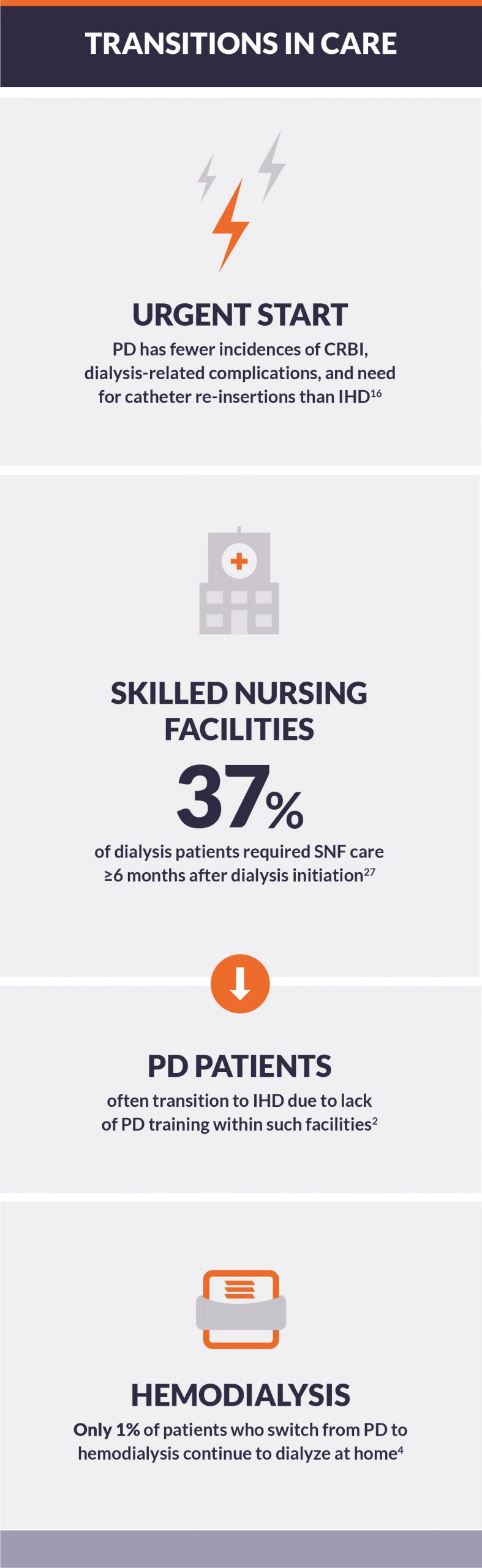
Learn MoreTransitions in care for peritoneal dialysis patients
Whether initiating a dialytic therapy, switching from one modality to another, or making a decision to commence palliative care, transitions introduce a risk of discontinuity in care.1 Patients on peritoneal dialysis (PD) transition away from PD for many reasons, including clinical complications due to multimorbidity, and PD-specific complications such as catheter malfunctions, peritonitis, and ultrafiltration. These complications can lead to hospitalization, as well as skilled nursing facility care, presenting risk of transitions from PD to in-center hemodialysis (IHD).
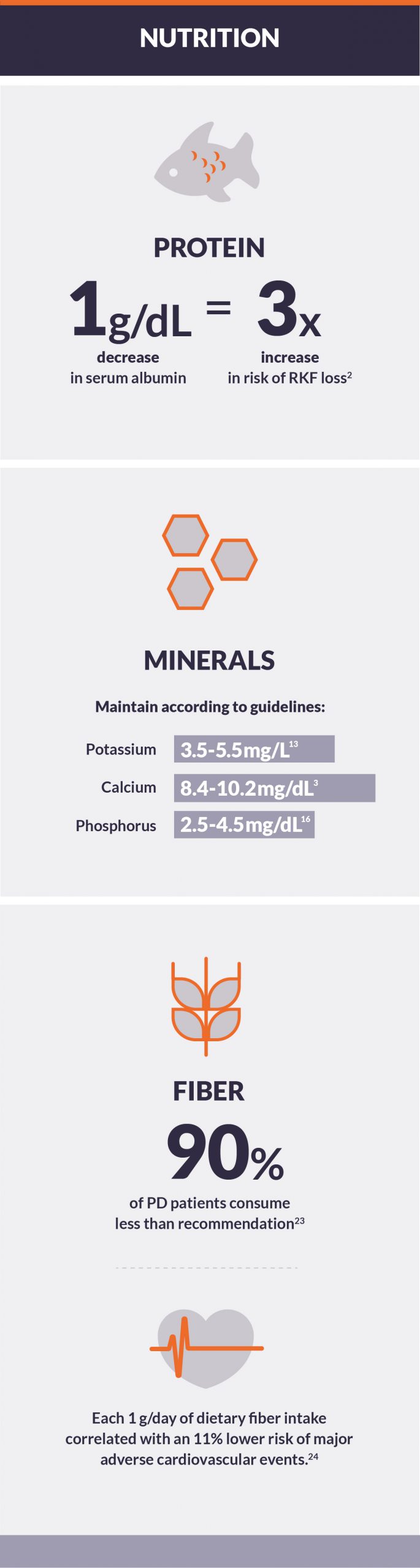
Learn MoreNutritional status concerns for peritoneal dialysis patients
Of end-stage renal disease (ESRD) patients starting dialysis, 20% have poor nutritional status, indicated by very low serum albumin (< 2.5 g/dL).1 Peritoneal dialysis (PD) is less likely to be the first dialysis modality with these patients due, in part, to peritoneal protein loss during PD.2 But while low serum albumin, calcium, and phosphorus levels may reflect poor nutritional status, they also may result from inappropriate treatment.3 Disturbed bowel habits, for example, may play a role in the accumulation of uremic toxins.
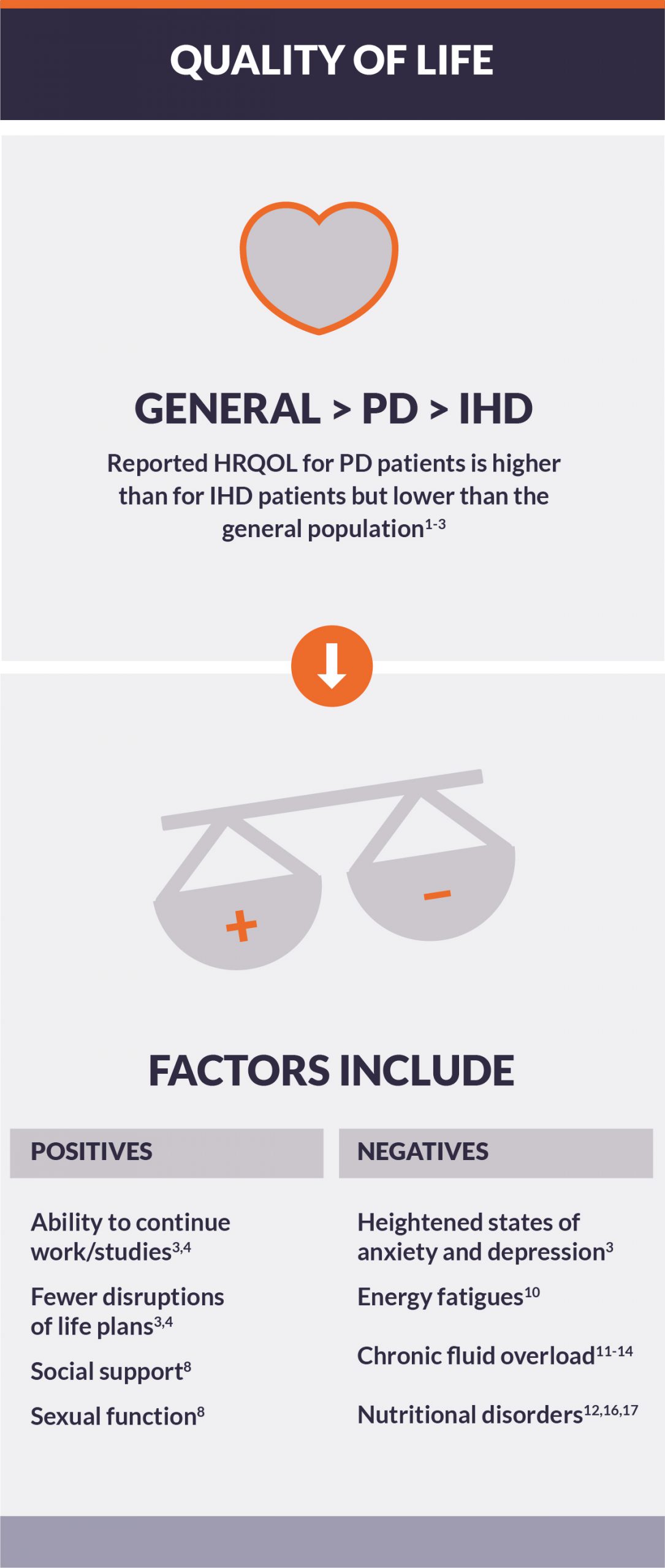
Learn MorePeritoneal dialysis and health-related quality of life
Research has shown that patients on dialysis rate their health-rated quality of life (HRQOL) much lower than the general population.1,2 This is a concern, as diminished HRQOL is associated with increased risks of morbidity and mortality.3 While those using peritoneal dialysis (PD) reported their HRQOL as much higher than patients receiving conventional in-center hemodialysis (IHD),4 frequent hospitalizations and administering daily treatments can increase the burden of therapy, impacting patients and care partners alike.
Learn MoreIncreasing transplantation incidence
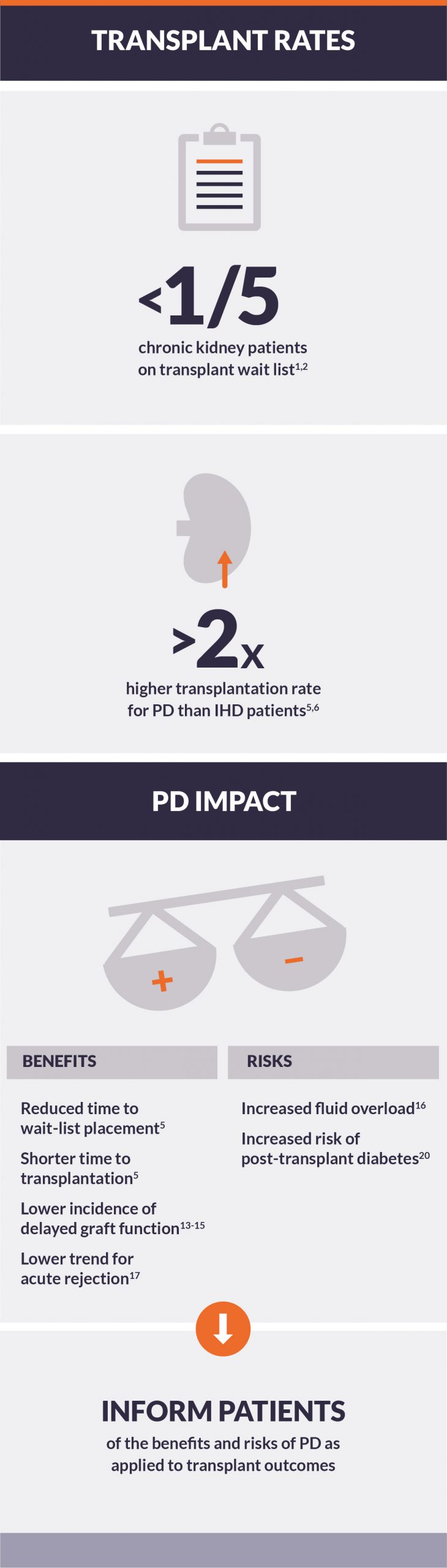
Of the more than 500,000 patients on chronic dialysis in the US, less than one-fifth are active on the kidney transplant waiting list —despite broad agreement on the economic and quality-of-life benefits to transplant.1-3 Several factors influence this, including graft availability, wait time, and post-transplant viability.
Wait-list placement time and transplantation incidence
Most incident ESRD patients are prescribed conventional hemodialysis (IHD) over peritoneal dialysis (PD) in the United States.1 This is despite findings that PD may be a better pre-transplant dialysis modality.
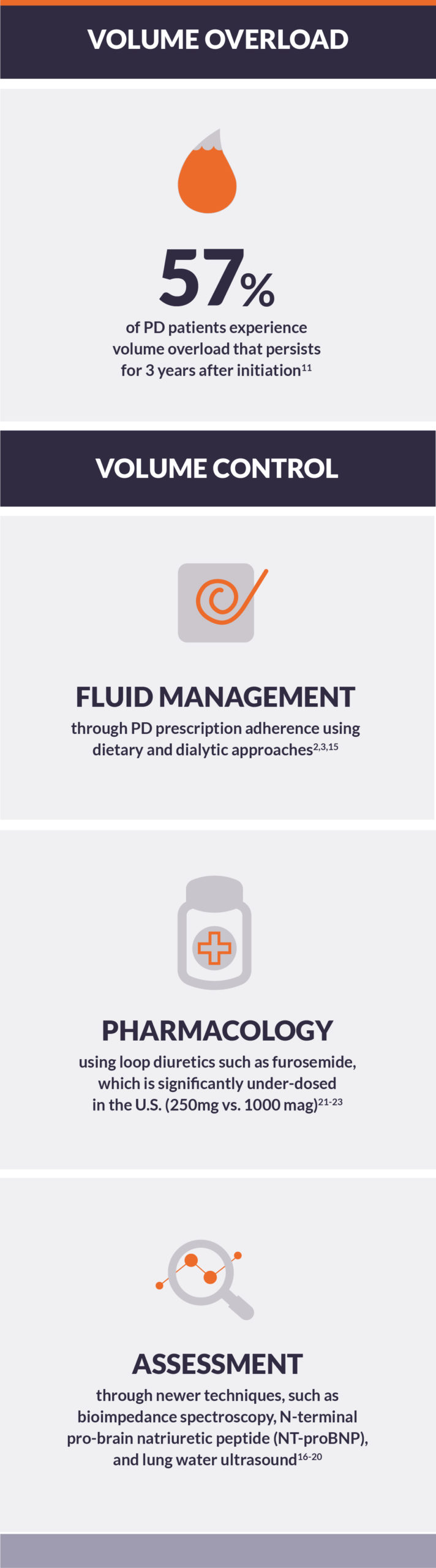
Learn MoreVolume control and peritoneal dialysis
The very nature of peritoneal dialysis (PD) avoids many of the complications inherent in thrice-weekly in-center hemodialysis (IHD),1 including allowing for gentle ultrafiltration during all hours—day and night.2 Volume overload, however, is common with PD and should be addressed.3
Avoiding interdialytic symptoms associated with IHD
High rates of ultrafiltration during hemodialysis sessions are associated with higher rates of cardiovascular death and hospitalization, as well as increased incidence of intradialytic hypotension and longer post-dialysis recovery time.
Learn MorePeritoneal dialysis and residual kidney function
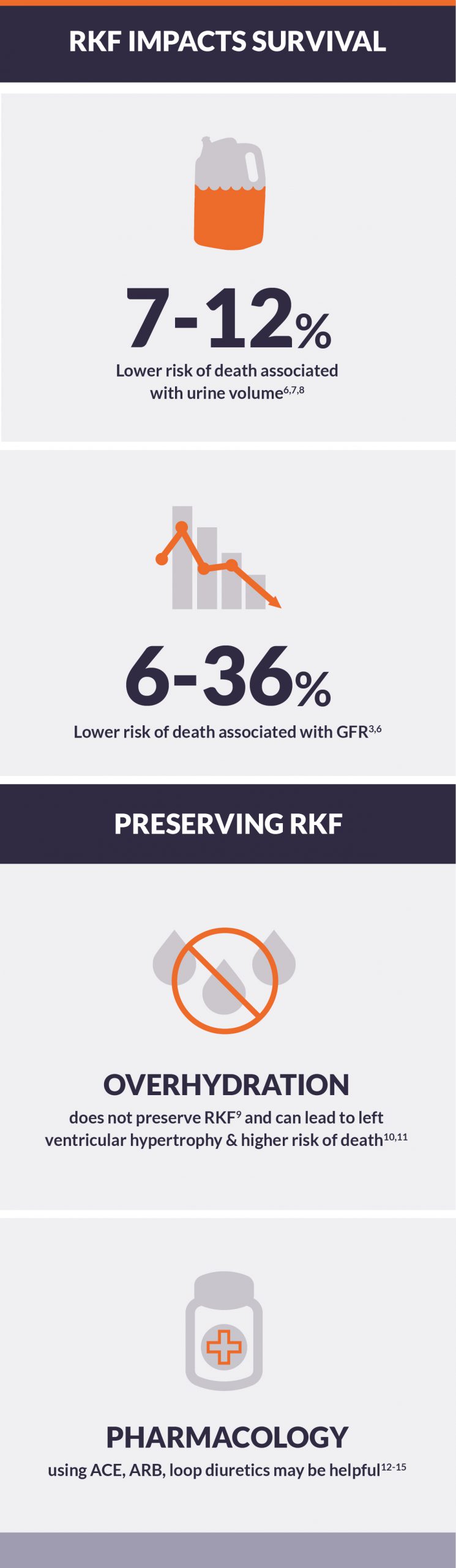
Many peritoneal dialysis (PD) patients initiate therapy with some residual kidney function (RKF). The importance of preserving this RKF and minimizing the potential for further kidney injury cannot be overstated.1,2,3 It is well established that end-stage kidney disease patients with substantial RKF live longer. Both glomerular filtration rate (GFR) and urine volume have been associated with improved survival in numerous studies.3
Preservation of RKF and survival
RKF in peritoneal dialysis patients appears to be more strongly associated with survival than peritoneal clearance.
Learn More