Nutritional status concerns for peritoneal dialysis patients
Of end-stage renal disease (ESRD) patients starting dialysis, 20% have poor nutritional status, indicated by very low serum albumin (< 2.5 g/dL).1 Peritoneal dialysis (PD) is less likely to be the first dialysis modality with these patients due, in part, to peritoneal protein loss during PD.2 But while low serum albumin, calcium, and phosphorus levels may reflect poor nutritional status, they also may result from inappropriate treatment.3 Disturbed bowel habits, for example, may play a role in the accumulation of uremic toxins.4 As a result, interventions should be implemented, such as monitoring of residual kidney function (RKF), nutritional supplements, and proper prescriptions.3,5
Advocating the use of PD in patients with low serum albumin
Decreased protein and energy intake due to anorexia, increased protein catabolism, decreased anabolism, chronic inflammation, metabolic acidosis, and hormonal imbalances have all been linked to protein energy wasting as etiological factors.6 Plus, protein catabolism, increased protein losses through the PD technique, and decreased synthesis of albumin lead to a state of negative nitrogen balance and muscle wasting.6 Studies suggest that maintaining higher serum albumin levels may delay RKF loss in PD patients, which is of great importance given the association it has with reduced mortality.2,7
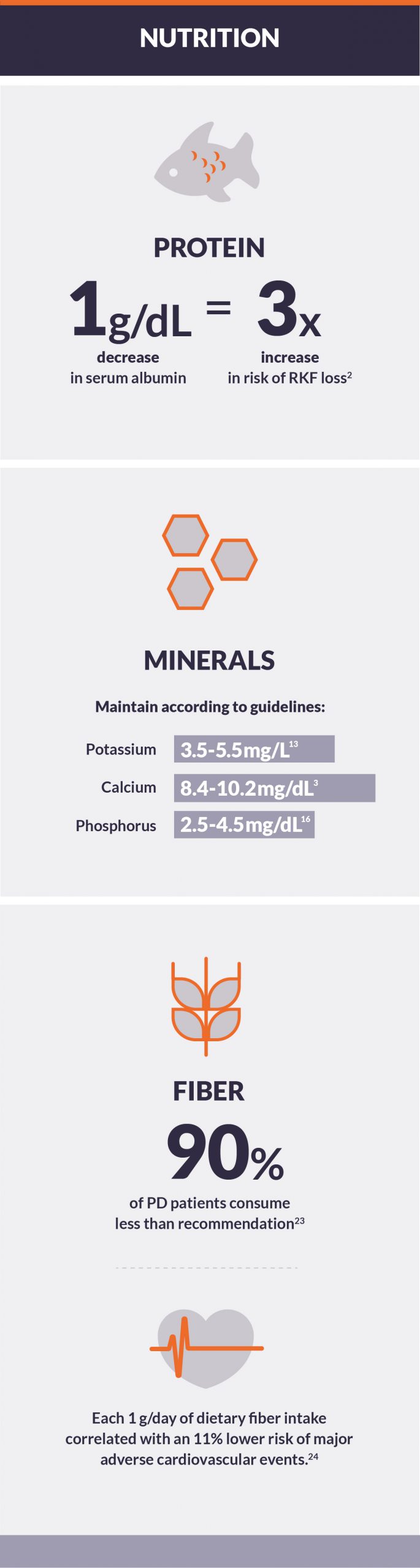
- Every 1 g/dL decrease in serum albumin has been associated with an over threefold increased risk of RKF loss.2
- Even in patients with low serum albumin, PD is associated with an 18% lower risk of mortality than conventional HD.1
- Whey protein has been shown to achieve adequate daily protein intake, as well as improvements in weight, BMI, skin fold measures, serum urea, and nPCR levels.8
- Use of probiotics may decrease C-reactive protein levels and interleukin 6, while increasing serum albumin levels in patients on PD.9
Strategies should be employed to better manage mineral and bone disease in PD
Observational studies demonstrate independent, U-shaped relationships between serum levels of potassium, calcium, and phosphorus and mortality.3,10–12
- Guidelines suggest serum potassium levels in patients undergoing PD should be maintained between 3.5 and 5.5 mg/L.13
- Hyperkalemia was found in 50.7% of PD patients.14
- Hypokalemia was found in 23.9% of PD patients.14
- Typically, serum calcium levels should be maintained between 8.4 and 10.2 mg/dL.3
- 1.9% of PD patients had serum calcium levels greater than 10.2 mg/dL15
- 23.1% of PD patients had serum calcium levels less than 8.4 mg/dL15
- Guidelines suggest maintaining serum phosphorus levels between 2.5 and 4.5 mg/dL.16 In clinical practice, most physicians and dietitians strive to maintain pre-dialysis phosphorus between 3.0 and 5.5 mg/dL.3
- 71.6% of patients on PD had serum phosphorus levels greater than 4.5 mg/dL.15
- 42.4% of patients on PD had serum phosphorus levels greater than 5.5 mg/dL, indicating a clear opportunity for improvement in serum phosphorus control.15
Energy absorption and glycemic control can be controlled with the right prescription
Glucose is absorbed during peritoneal dialysis, with the amount of energy intake dependent on factors that include concentration of the solution used, PD modality and prescription, and the patient’s serum glucose levels.16
- The majority of PD patients in the U.S. perform 4-5 continuous cycling PD exchanges, using approximately 12 liters of dialysate.17 As a result, anywhere from 430 to 1,250 calories are absorbed daily.18
- Using an icodextrin-based solution has shown a marked reduction in glucose absorption and insulin needs compared to use of a 4.25% glucose solution; however, only a negligible difference when compared to use of a 2.5% glucose solution.19
High fiber diets help with common gastrointestinal issues in PD patients
Gastrointestinal issues are common in dialysis patients, with 62% of PD patients reporting them.20 Constipation can lead to long drains, shortened dwell times, machine alarms, and technique failure.21 Studies have confirmed that increased fiber intake and the use of fiber supplements and/or stool softeners can improve bowel function without affecting biochemistry.9,22
- It has been reported that 90% of PD patients consumed less than the recommended fiber intake of 25 g/day, with a median of 12.2 g/day.23
- Increased dietary fiber intake can improve constipation commonly reported by PD patients.20
- In a study of 219 PD patients in China, each 1 g/day of dietary fiber intake correlated with an 11% lower risk of major adverse cardiovascular events.24
Conclusion
Maintaining a nutritional balance can help patients on PD be successful. The right prescription can help manage serum albumin levels, bone and mineral disease, and caloric absorption. With GI issues common for PD patients, a high fiber diet can help—including significantly reducing poor dialysis efficiency and technique failure without affecting a patient’s overall biochemistry.