Peritonitis in peritoneal dialysis
Peritonitis is the most serious infectious complication associated with peritoneal dialysis (PD) therapy.1 Peritonitis rates have shown significant improvement over the years, with recent data reporting infection-related hospitalizations experienced by 16% of peritoneal dialysis patients.2 However, infection-related deaths accounted for 10% of PD patients versus 7% of conventional hemodialysis (IHD) patient deaths.3 Secondary complications of PD-related infections significantly compromise long-term use of the peritoneal membrane, patient well-being, and longevity.4-6 For the long-term success of PD patients, focused strategies to reduce risk and to ensure therapeutic antibiotic dose are essential.7-9
Factors associated with increased and decreased risk of peritonitis
Exit-site and catheter-tunnel infections are major predisposing factors to PD-related peritonitis.10 A number of improvements in PD over the past several years, including better disconnect systems, have resulted in decreased peritonitis rates.11 Training, retraining, and home visits are necessary to guarantee training efficacy.12-14 Potential sources for increased risk should also be considered.
- Increased exposure to glucose in combination with loss of residual kidney function (RKF) increased peritonitis risk.5,16,17
- Obese patients have higher risk of complications than non-obese patients and may be biased toward increased peritoneal infections.15
- Use of immunosuppressive drugs and glucose exposure per 100 g/24h at 6-months was associated with a nearly a 3.5 and >twofold increased risk of peritonitis respectively.16
- Preservation of RKF and higher serum albumin decreased the risk of peritonitis by 47% and 11% respectively.16
- Center-level predictors of lower peritonitis rates included smaller center size and high proportion of patients on PD.18,19
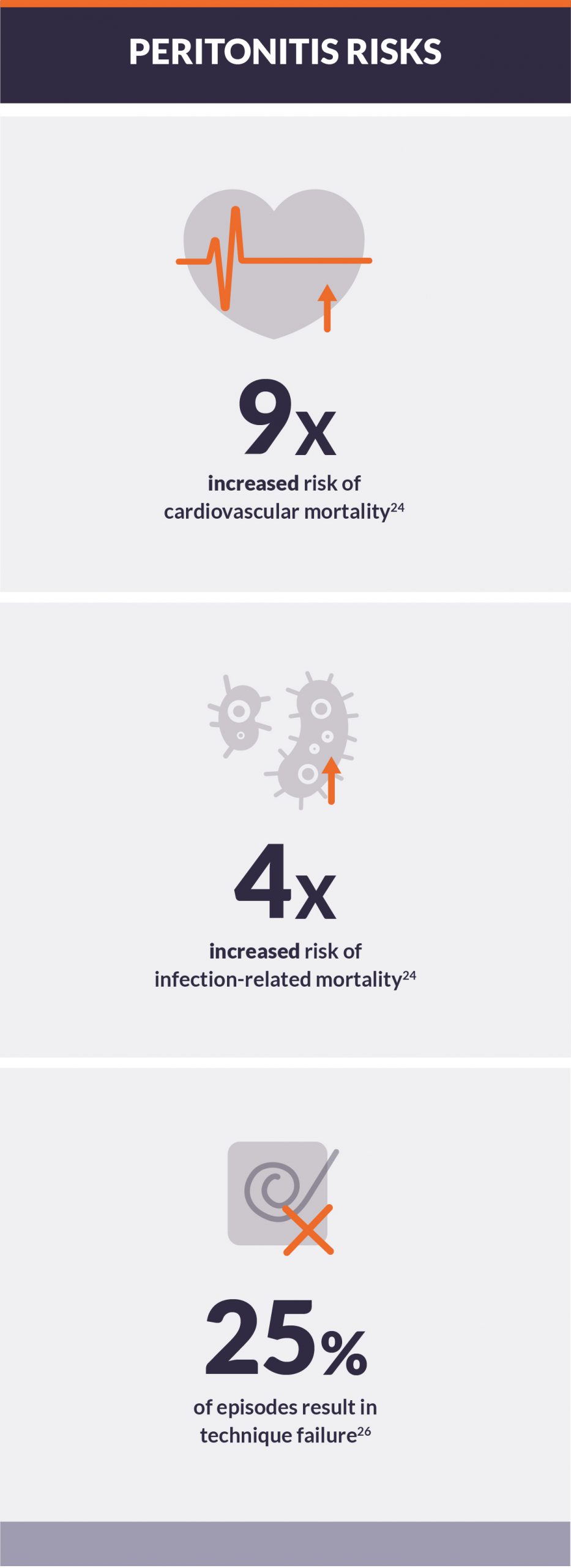
Association with all-cause, infection-related, and cardiovascular-related mortality
Observational studies have shown a range of between 3% and 10% of PD-related infections result in death.20-23 An episode of peritonitis has been reported to be a cofactor for mortality in an additional 16% of affected patients.24
- In patients on PD therapy for over 2 years, peritonitis was independently associated with 95% increased risk of all-cause mortality, ninefold increased risk of cardiovascular mortality, and near 4-fold increased risk of infection-related mortality.24
- Early onset peritonitis (EOP), defined as peritonitis within 6 months of initiating PD, was independently and multivariately associated with increased risk of technique failure and mortality.15
- EOP was independently associated with a >2-fold increased risk of mortality and technique failure.25
- Multivariate analysis did not reduce risk dramatically; risk remained between 1.7 and 2 times higher with occurrence of EOP.25
Peritonitis and technique survival
Since peritonitis is one of the more common complications of PD, it has caused patients to switch from this modality to hemodialysis.
- In an analysis of 855 episodes of peritonitis in 435 PD patients, 25.2% of the episodes resulted in technique failure.26
- Renal clearance of antibiotics should be paid attention to, and the monitoring of antibiotic levels is paramount to ensure therapeutic dose is achieved.7-9
- Peritonitis in patients with creatinine clearance of 0-5 mL/min had 6.8 higher odds of treatment failure than episodes experienced by anuric participants.8
- Episodes experienced by participants with creatinine clearance 0-5ml/min also had significantly higher odds; 2.9 increased odds of treatment failure than episodes experienced by anuric participants.8
- The odds of relapse and recurrent peritonitis among participants with creatinine clearance >5 ml/min was also 7 times higher compared with anuric participants.8
Conclusion
Peritonitis was independently associated with increased risk of all-cause, cardiovascular, EOP, and infection-related mortality. The duration of peritoneal dialysis also has an increased risk of mortality combined with infection. Focused strategies to reduce peritonitis risk, prompt and appropriate management, and measures to assure therapeutic antibiotic dosing are essential for the long-term success of PD in all patients.7