Intensive hemodialysis reduced post-treatment fatigue and recovery time
Hemodialysis can be difficult to tolerate. Common complications are intradialytic hypotension and long recovery time after treatment.1 Intradialytic hypotension may be caused by aggressive ultrafiltration in response to interdialytic weight gain, related to myocardial stunning and cardiac arrhythmias, and is associated with increased risk of death.2 Long recovery times may impair physical and mental function and decrease qualify of life.3 Patients and caregivers rank fatigue more highly than any other problem, including life expectancy.4
Studies show that intensive hemodialysis is associated with reduced intradialytic hypotension and recovery time
Due to lower ultrafiltration volume and/or ultrafiltration rate, intensive hemodialysis may reduce intradialytic blood pressure variability.
- In the Frequent Hemodialysis Network trials, short daily and nocturnal schedules reduced per-session probabilities of symptomatic intradialytic hypotension by 20% and 68%, respectively, relative to three sessions per week.5,6
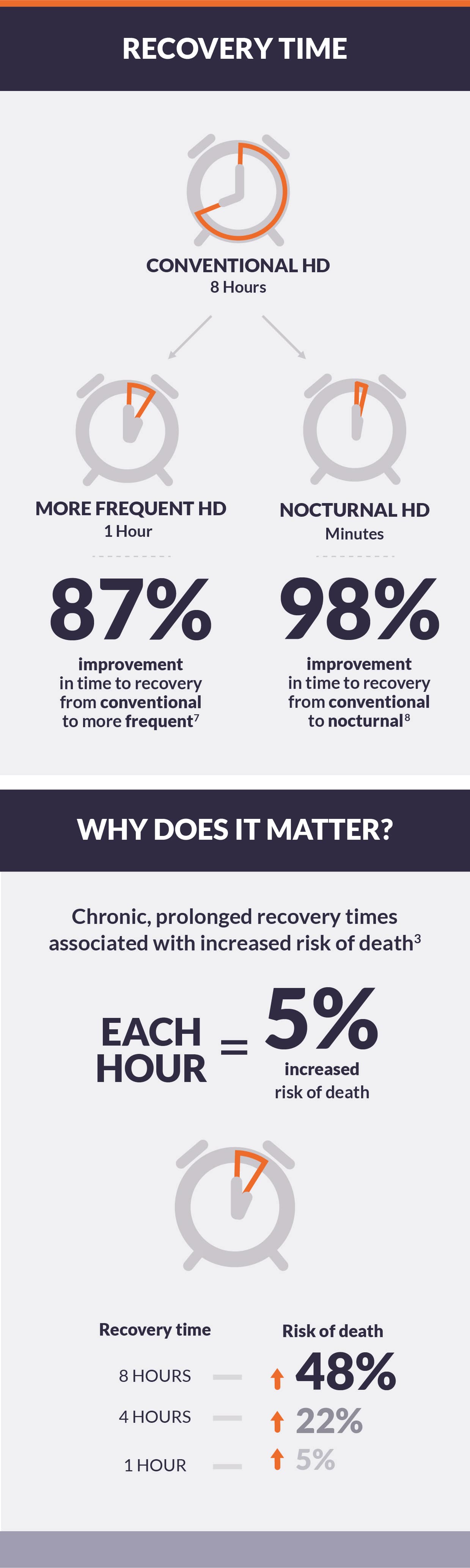
- In the Following Rehabilitation, Economics, and Everyday-Dialysis Outcome Measurements (FREEDOM), a prospective cohort study of short daily hemodialysis, mean post-dialysis recovery time was reduced after 12 months from eight hours to one hour.7
- Recovery time after nocturnal hemodialysis may be minutes in duration.8
Conclusion
Accumulated evidence shows that intensive hemodialysis may improve the tolerability of hemodialysis treatment by reducing the risk of intradialytic hypotension and dramatically lowering recovery time after each session. Therefore, intensive hemodialysis may address some of the issues cited by patients as important outcomes and may improve the patient centeredness of dialysis delivery.