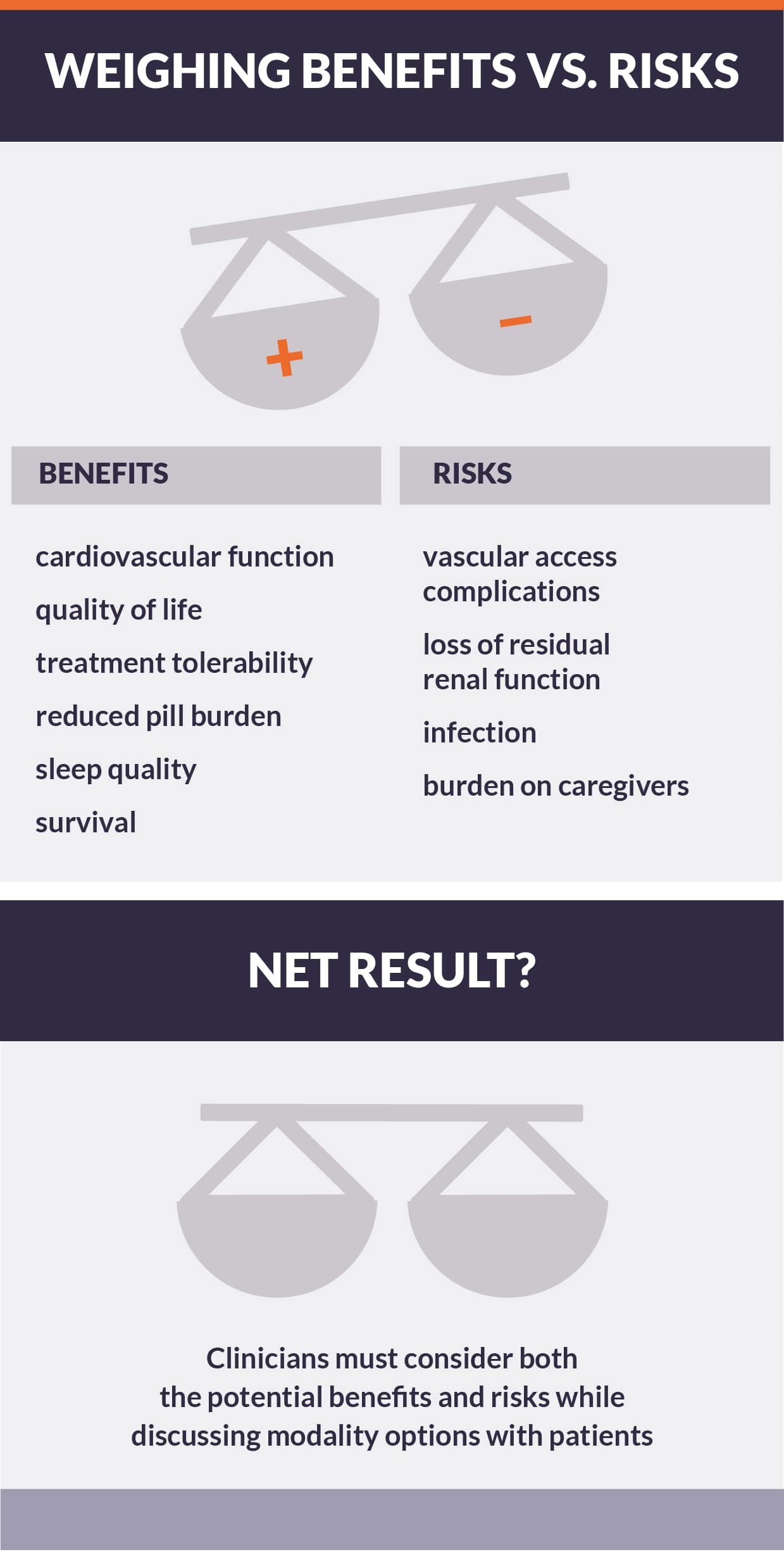
A question of balance: Benefits vs. risks of intensive hemodialysis
Although intensive hemodialysis may address important clinical problems, increasing treatment may introduce risks pertaining to six domains: vascular access complications, infection, mortality, loss of residual renal function, solute balance, and patient and care partner burden.
Trials have shown increased access complications and infection
- In the Frequent Hemodialysis Network (FHN) trials, short daily and nocturnal schedules increased incidence of access complications, most commonly due to infection, although incidence of access loss was not statistically elevated. 1
- Observational studies regarding vascular access complications are mixed.2,3
- Excess risk may be catalyzed by poor infection control practices in the home setting, where intensive hemodialysis is typically delivered, but with an assumption of fixed probability of bacterial contamination per cannulation, greater treatment frequency necessarily increases risk of infectious complications.4,5
Data regarding mortality are equivocal
- With extended follow-up of subjects in the FHN trials, short daily hemodialysis was associated with lower risk of death, relative to conventional hemodialysis, while nocturnal hemodialysis was associated with higher risk. However, the FHN trials were never powered to assess mortality and suffer from significant limitations, including substantial crossover in treatment schedules after 12 months of follow-up.5,6,7
- In many—but not all—observational studies, short daily hemodialysis has been associated with lower risk than both in-center hemodialysis and peritoneal dialysis; however, observational studies are subject to unmeasured confounding.8,9
Increased treatment may increase loss of residual renal function, burden on caregivers, and may deplete solutes
- Intensive hemodialysis has been reported to accelerate the loss of residual renal function in incident dialysis patients with substantial urine output, relative to conventional hemodialysis, and may deplete solutes (e.g., phosphorus), to the extent that supplementation is necessary.10,11,12
- Intensive hemodialysis may increase burden on patients and caregivers, possibly leading to technique failure.13,14
Conclusion
Ultimately, intensive hemodialysis is not a panacea for kidney failure. In spite of the benefits of intensive hemodialysis on cardiovascular function, health-related quality of life, and treatment tolerability, intensive hemodialysis may introduce specific risks pertaining to vascular access complications, infections, loss of residual renal function, and increased burden on caregivers. As much as enthusiasm for the clinical effects of intensive hemodialysis may be warranted, patients and clinicians must consider the potential disadvantages of dialyzing more frequently, consider both the potential benefits and risks of treatment, and prepare for possible adverse effects.