Peritoneal Dialysis in the United States Amidst COVID-19
Opinion article
Clinical Practice Learnings with Potential Post-Pandemic Application
The world is amidst a public health crisis related to the COVID-19 pandemic. COVID-19 will remain a primary healthcare concern until a vaccine and effective medications are discovered, which may take many more months.1 End-Stage Renal Disease (ESRD) patients are at particularly high risk of this coronavirus infection because of chronic immunocompromised state, a high burden of co-morbid conditions, and high healthcare utilization.2,3 In the US, the first two COVID-19 related deaths occurred in in-center hemodialysis (ICHD) patients, who are at a higher risk of viral transmission because of limited ability to socially distance, interactions with other patients and healthcare staff, and frequent need for transportation to and from dialysis treatments.4 Home dialysis patients are at an obvious advantage by dialyzing at home, where they can better adhere to social distancing recommendations. They also require fewer visits to dialysis facilities and interactions with healthcare workers, which potentially lowers their risk of COVID-19 infection.
Peritoneal Dialysis before COVID-19
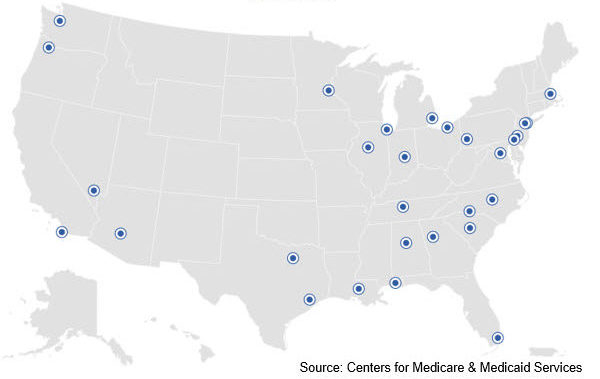
ESRD beneficiaries represent approximately 2% of the Medicare population but account for over 7% of overall Medicare spending.5,6 Over the last decade, Centers for Medicare and Medicaid (CMS) has taken several measures to transition from fee-for-service to a value-based payment model, to reduce overall healthcare costs while improving care and clinical outcomes for ESRD patients. In 2011, the Prospective Payment System, also called the “bundle,” was implemented to rein in costs for the ESRD patients. As an incentive, CMS made the bundled payments for peritoneal dialysis (PD) equivalent to ICHD treatments and started payments for PD from the first day of dialysis initiation.7 In 2016, the Centers for Medicare and Medicaid Innovation (CMMI) developed the ESRD Seamless Care Organizations (ESCOs), which was initially a demonstration project and expanded a few years ago to 33 participants.8
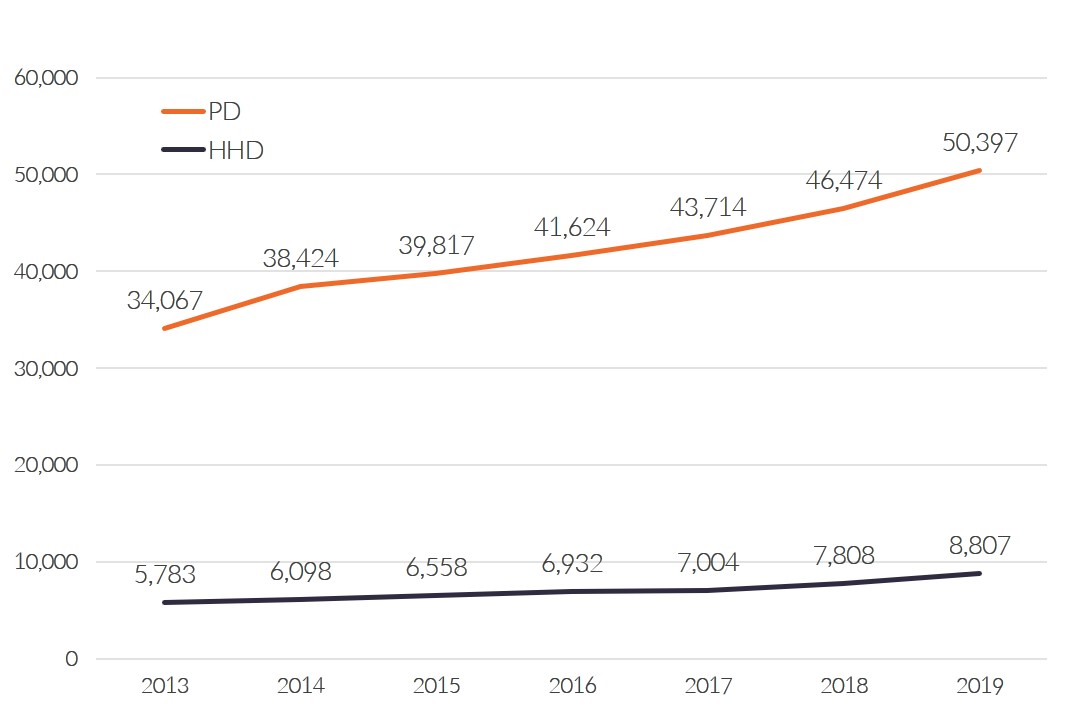
PD is a very effective dialysis modality and maintains better 3-year survival, while being approximately $14,000 per patient per year cheaper than ICHD.9,10 Consequently, under these value-based pay for performance models, PD in the U.S. increased significantly since 2011.11
Figure 1: Growth of Home Dialysis amongst 10 largest US dialysis providers
Value-based health care is here to stay and will impact future delivery of care to the ESRD population. On July 10, 2019, President Donald Trump issued an Executive Order, referred to as the Advancing American Kidney Health Initiative, which, among many things, outlined the goal to have 80% of new ESRD patients either receive home dialysis or a kidney transplant by 2025.12
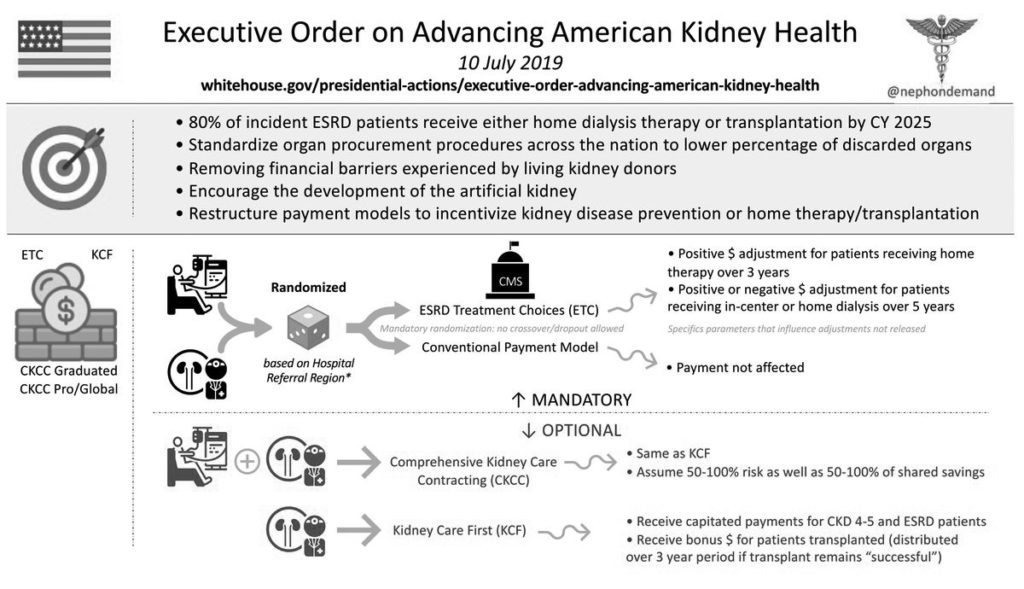
To coincide with the Executive Order, CMS proposed five value-based models with the objective to increase home dialysis and transplant in the next 5 years. The mandatory ESRD Treatment Choices model proposing two payment adjusters, the Payment Performance Adjustment (PPA) and the Home Dialysis Payment Adjustment (HDPA), both designed to increase home dialysis and transplant. The proposed PPA is scheduled to begin July 2021. The HDPA was to begin in January 2020, and will likely to go into effect once the final rule is issued.13
Peritoneal Dialysis during the COVID-19 Pandemic
In the US, both PD and home hemodialysis (HHD) have been significantly impacted by the Pandemic. While we have seen continued increase in number of patients starting HHD treatments, there has been a significant decline in PD starts in the last three months.
The decline in chronic PD during the Pandemic may be due to several reasons:
- Reduced numbers of late chronic kidney disease (CKD) patients starting dialysis – which could be due to disruptions to nephrologists’ care of CKD patients in their offices – and in some cases, delaying dialysis starts until initiation is medically essential.
- Nephrologists may be experiencing a significantly increased workload and may be under tremendous stress during the Pandemic. This could result in some passivity towards home dialysis growth.
- Some hospitals initially deemed PD catheter placement as elective surgeries and stopped procedures to preserve PPE, free up hospital beds, and to reduce community spread of COVID-19. CMS released a statement that dialysis access procedures, including PD catheter placement, are not considered elective and should be considered a lifeline for dialysis patients. These guidelines have since been added to the American College of Surgeon Guidance for Surgical Care during COVID-19.14
- There was a significant reduction in the number of PD catheters placed, especially in patients who had a preexisting access for dialysis. While hospitals are resuming elective procedures, many have limited operating room availability for PD catheter placement.
- PD education was significantly impacted because many dialysis patient educators were learning how to provide modality education for CKD and ICHD patients remotely. Additionally, several Transitional Care Units (TCU) were hindered because of staffing issues or because the TCU had been converted to an isolation unit.
Post-Pandemic Peritoneal Dialysis
In contrast, we have seen a reemergence of PD for Acute Kidney Injury (AKI) in patients admitted to hospital systems in Metro New York and New Orleans where access to CRRT machines were limited. In these hospitals, PD catheters were percutaneously placed at the bedside by surgeons and interventional radiologists. Although still early, the outcomes of the placed PD catheters were very good with very little mechanical complications or peri-catheter leaks.15
In March 2020, CMS granted dialysis facilities several telehealth waivers under the Section 1135 of the Coronavirus Preparedness and Response Supplemental Appropriations (CARES) Act. CMS allowed increased access to telehealth to ensure that patients on home dialysis had ongoing, unhindered quality care from their nephrologists and care teams, without increasing their risk of contracting coronavirus infection.16
The COVID-19 Pandemic has accentuated the potential advantages of home dialysis for patients, nephrologists, and clinicians. This could lead to significant positive changes within a rapidly transforming dialysis industry, and further augment the efforts to increase the utilization of home dialysis in the US, especially among ICHD patients.
The familiarity of providers, clinicians, and patients with utilizing telehealth during the pandemic could be a catalyst for increased use of telehealth, virtual care, connected health technologies, and remote daily patient monitoring in the management of home dialysis patients.
The experience with Acute PD during the pandemic should improve nephrologists’ comfort with prescribing PD for AKI patients post-COVID-19. The outcomes with acute PD make it a viable alternative to hemodialysis for ICU patients needing renal replacement therapy for AKI. The experience with immediately starting PD after placement of a PD catheter in the hospital will hopefully lead to more urgent start PD for ESRD patients.
Furthermore, PD could become a preferred modality for incident ESRD patients receiving their first dialysis in the hospital.
Potential Risks
Not everyone will experience the reported benefits of home and more frequent dialysis. All forms of dialysis involve some risks. Peritoneal dialysis does involve some risks that may be related to the patient, center, or equipment. These include, but are not limited to, infectious complications.
Certain risks associated with home dialysis treatment are increased when performing independent dialysis because no one is present to help the patient respond to health emergencies.
Certain risks associated with home dialysis treatment are increased when performing nocturnal therapy due to the length of treatment time and because the patient and care partner are sleeping.