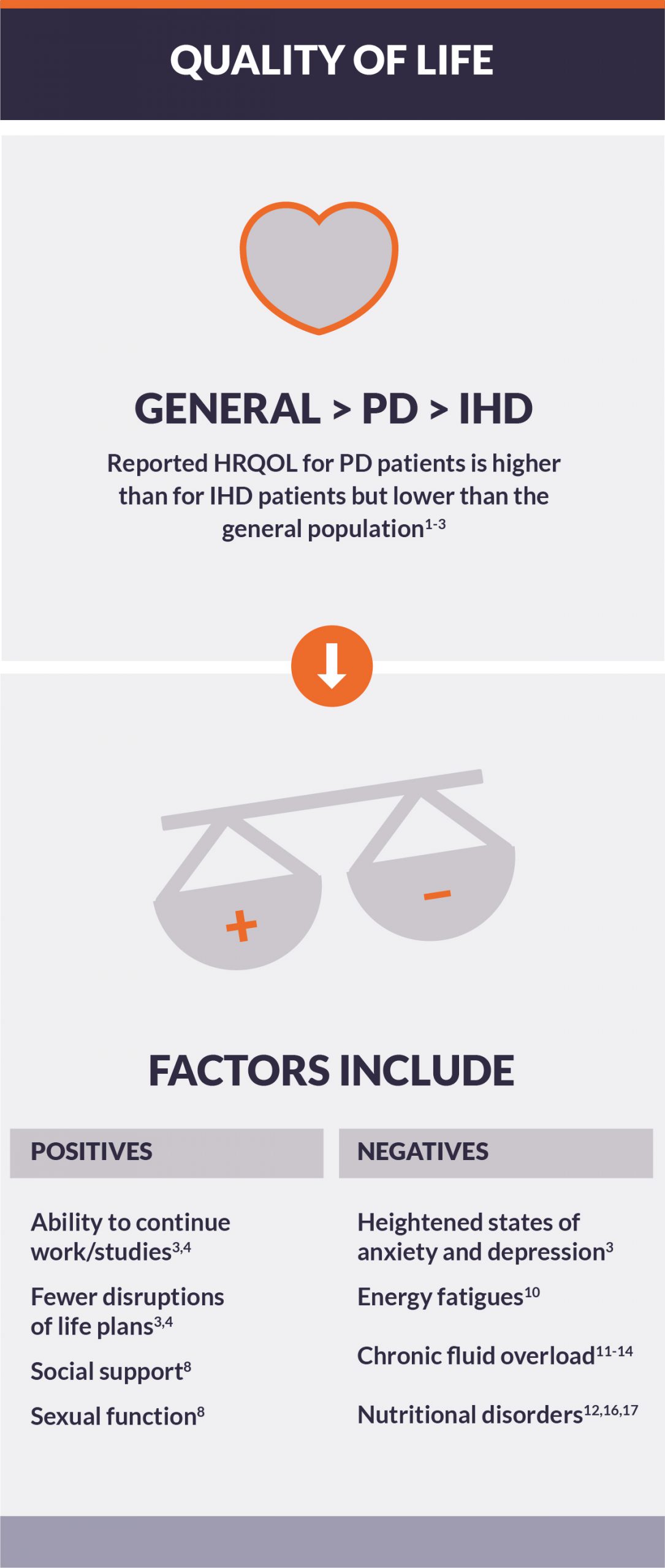
Peritoneal dialysis and health-related quality of life
Research has shown that patients on dialysis rate their health-rated quality of life (HRQOL) much lower than the general population.1,2 This is a concern, as diminished HRQOL is associated with increased risks of morbidity and mortality.3 While those using peritoneal dialysis (PD) reported their HRQOL as much higher than patients receiving conventional in-center hemodialysis (IHD),4 frequent hospitalizations and administering daily treatments can increase the burden of therapy, impacting patients and care partners alike.2,5
Factors associated with greater quality of life (QOL) in PD patients
PD has been associated with greater HRQOL during the initial period after dialysis and for up to two years as compared to IHD, even after adjusting for clinical and socioeconomic characteristics.8
- Scores of three clinical domains (effects of kidney disease, burden of kidney disease, and dialysis staff encouragement) and two socioeconomic domains (sexual function and dialysis staff encouragement) were higher in patients on PD compared with those on IHD at one and two years after dialysis initiation.8
- Patients with stage 5 chronic kidney disease or ESRD treated with PD had better general HRQOL than IHD patients, specifically in subdomains of physical functioning, role limitations due to emotional problems, side effects, and burden of kidney disease.9
- A separate analysis of modified kidney disease QOL survey data showed that although PD patients experienced identical dialysis-related symptoms as IHD patients, they were to a lesser degree.4 Highly affecting parameters were the ability to continue work or studies, fewer disruptions of life plans, and the will to live.4
Factors associated with diminished QOL in PD patients
Initiation of renal replacement therapy has a strong impact on HRQOL in comparison with other stages of chronic kidney disease.10
- Emotional aspects of HRQOL were significantly associated with heightened states of anxiety (26.6%) and depression (27%).10
- Lower physical role scores were significantly and independently associated with lower emotional role, energy fatigue, and social function scores.10
Chronic fluid overload, inflammation, malnutrition, and multimorbidity (commonly, cardiovascular disease and diabetes mellitus) are common factors negatively affecting PD patients’ HRQOL and increasing their risk of death.11-14
- Overhydration was independently associated with lower physical component (PCS) and mental component scores (MCS), and kidney disease component scores.8,15
- Lower HRQOL was significantly associated with lower serum albumin and sodium levels, higher BMI, and lower subjective global assessment.12,16,17
The most affected QOL dimensions were effects of the disease, burden of the disease, occupational status, sleep, and satisfaction.18
More strategies are needed to reduce burden of care on patients and caregivers
Patients on dialysis often need caregiving and assistance from family members and/or others to attend hospital visits and supervise therapy administration. This places a considerable burden on caregivers, which can in turn influence their QOL.19
- The physical component of the QOL questionnaire was negatively associated with the number of hospital admissions over the previous year and positively associated with social support.3 Lower mean scores of HRQOL physical functioning domain have been associated with increased risk of death.12,20
- Compared to national norms, caregivers and dialysis patients tended to have poor physical HRQOL but normal MCS; lower caregiver MCS revealed nearly a sevenfold correlation to dialysis duration and tenfold for burden of kidney disease.21
- Caregivers also tended to have lower physical HRQOL if their loved one had higher social HRQOL, and lower mental health-related QOL during the early stage of the patient’s dialysis treatment and when patients experienced low disease-targeted QOL.21
Conclusion
As compared to IHD, PD patients have greater autonomy and better HRQOL. Social support is observed to be a key factor in perceived QOL. Greater symptomology corresponded to worse HRQOL and to perceiving the disease as a burden. The worse the HRQOL, particularly in PCS domains, the more a lower PCS should be considered a predictor of death.