Transitions in care for peritoneal dialysis patients
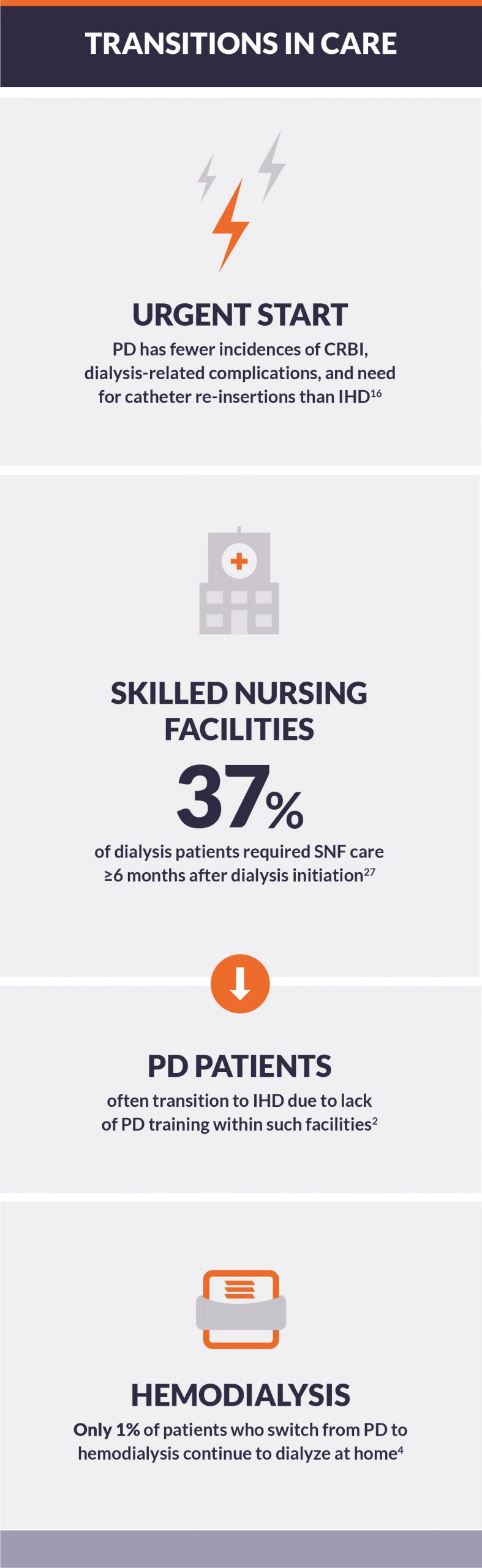
Whether initiating a dialytic therapy, switching from one modality to another, or making a decision to commence palliative care, transitions introduce a risk of discontinuity in care.1 Patients on peritoneal dialysis (PD) transition away from PD for many reasons, including clinical complications due to multimorbidity, and PD-specific complications such as catheter malfunctions, peritonitis, and ultrafiltration. These complications can lead to hospitalization, as well as skilled nursing facility care, presenting risk of transitions from PD to in-center hemodialysis (IHD).1,2 Unplanned IHD start is a common problem in patients transferred from PD.3 Only slightly more than 1% of patients who switch from PD to hemodialysis continue to dialyze at home.4
Incident PD referrals and successful catheter placement
Lack of patient preparedness and nephrology care prior to initiating dialysis are associated with lower survival and higher morbidity, regardless of dialysis modality.5-7 The success of PD as renal replacement therapy hinges on the patient possessing a functional peritoneal access.8 PD catheter insertion by a competent operator is necessary to affect safe and timely initiation of therapy.9-12
- Improper insertion of a catheter can lead to malposition, catheter-associated infection, technique failure, and/or all-cause mortality.9
- In a survey of surgery residency programs, 82% of respondents provided training in PD catheter placement, yet most surgeons only placed 2 to 5 catheters during residency.13
- One study showed an acceptable learning curve by an operator was achieved after 23 percutaneous procedures.14
- Catheter placement experience speaks volumes: centers that place more PD catheters per year have less frequent adverse events and shorter lengths of stay.12
Planned-start versus urgent-start PD have similar long-term outcomes
PD could be a better approach in an unplanned, new-to-dialysis patient compared to IHD.15 As compared to urgent-start IHD via a central venous catheter, urgent-start PD (USPD) has significantly fewer incidences of catheter-related bloodstream infections (CRBI), dialysis-related complications, and need for dialysis catheter re-insertions, and comparable short-term outcomes to urgent-start IHD and conventional PD.16 A well-trained PD team, standardized catheter insertion procedure, carefully designed initial PD prescription, and comprehensive follow-up care are reported to be essential for a successful urgent-start PD program.17
- Dialysis catheter placement within the urgent-start timeframe is limited by the capacity of a healthcare facility to support rapid placement of PD catheters, initiate PD treatment for urgent-start patients, and train patients on short notice.18
- Compared to planned-start PD, urgent-start PD is associated with a higher risk of leak and catheter migration. Proper placement technique, the use of purse-string sutures, and appropriate USPD prescriptions mitigate the risk of these complications.19
- Although there are more observations of urgent-start PD catheter mechanical dysfunctions, peritonitis, exit-site infection, or PD technique survival have been shown to be similar in urgent-start and planned-start PD patients.20
- Peritonitis and exit site rates of infection were 1:319 and 1:159 patient-months respectively, and no statistically significant difference in infection rates were observed between urgent-start vs. non-urgent-start PD patients.19
- No difference between planned-start and urgent-start groups has been shown in time-to-first complication, mean days-to-catheter removal, and overall patient survival at 12 months.21
- Urgent-start PD patients experienced a fivefold lower risk of 30-day, dialysis-related complications compared to urgent-start IHD patients.22
Hospitalizations and episodes of non-dialysis-related healthcare
The number of hospitalization days are 8% higher in PD compared to IHD; of these, 81% are non-dialysis-related.23
- Only 19% of hospitalizations in dialysis patients were dialysis-related, irrespective of dialysis modality.24
- Causes of non-dialysis-related hospitalizations in PD patients included 28% due to cardiovascular disease/complications, 16% infection, 11% elective surgery, and 20% “other unrelated”.24
- Cardiac issues accounted for 50% of admissions in the ICU for patients on PD with most patients having more than one diagnosis upon ICU admission.25
- Loss of lean body mass in PD patients can result in dry weights being set too high, possibly resulting in overhydration and risk of hospitalization for volume overload.26
Increased risk of PD technique failure during in-patient care and home dialysis upon PD completion
Numerous hospitals lack the ability to care for patients on PD, including trained staff, nephrologists, and stocked home dialysis supplies.2 This is also problematic in skilled nursing facilities (SNF). Patients on PD requiring SNF care are often transitioned to IHD due to lack of PD nurse training within a SNF and no provision for a SNF to offset costs of nurse training required for PD patient care.2
- Dialysis patients are at high risk of transitioning to long-term care facilities; ≥6 months after dialysis initiation, 37% of dialysis patients required SNF care.27 And, the risk of dialysis patients transitioning to a SNF increases if additional comorbidities are present.28
- Chronic PD patients rarely stayed on a home dialysis modality if transition away from PD became necessary.4
- One in six patients who started on PD switched to IHD within one year of initiation.4
- Only 521 out of nearly 33,000 PD patients switched from PD to home hemodialysis within six years of initiation.4
Conclusion
The transition onto dialysis remains an important milestone for patients with end-stage renal failure. A smooth transition from chronic kidney disease to PD initiation with prior preparation and planning is associated with better short- and long-term results. It allows an individual to be both physically and psychologically readied for the potential rigors of renal replacement therapy. Transitions in care while undergoing dialysis are critical to patient success at home, and to reduce hospitalizations and long-term care facility use, both of which present increased risk of PD technique failure.