Volume control and peritoneal dialysis
The very nature of peritoneal dialysis (PD) avoids many of the complications inherent in thrice-weekly in-center hemodialysis (IHD),1 including allowing for gentle ultrafiltration during all hours—day and night.2 Volume overload, however, is common with PD and should be addressed.3
Avoiding interdialytic symptoms associated with IHD
High rates of ultrafiltration during hemodialysis sessions are associated with higher rates of cardiovascular death and hospitalization, as well as increased incidence of intradialytic hypotension and longer post-dialysis recovery time.4–9
- The concept of an interdialytic gap, along with all its associated complications, is often eliminated because the majority of PD is performed daily.2
- PD may be a more effective therapy for patients who exhibit intolerability to the intermittency of hemodialysis due to heart failure comorbidities, whether in the facility or at home.10
PD and associated volume overload
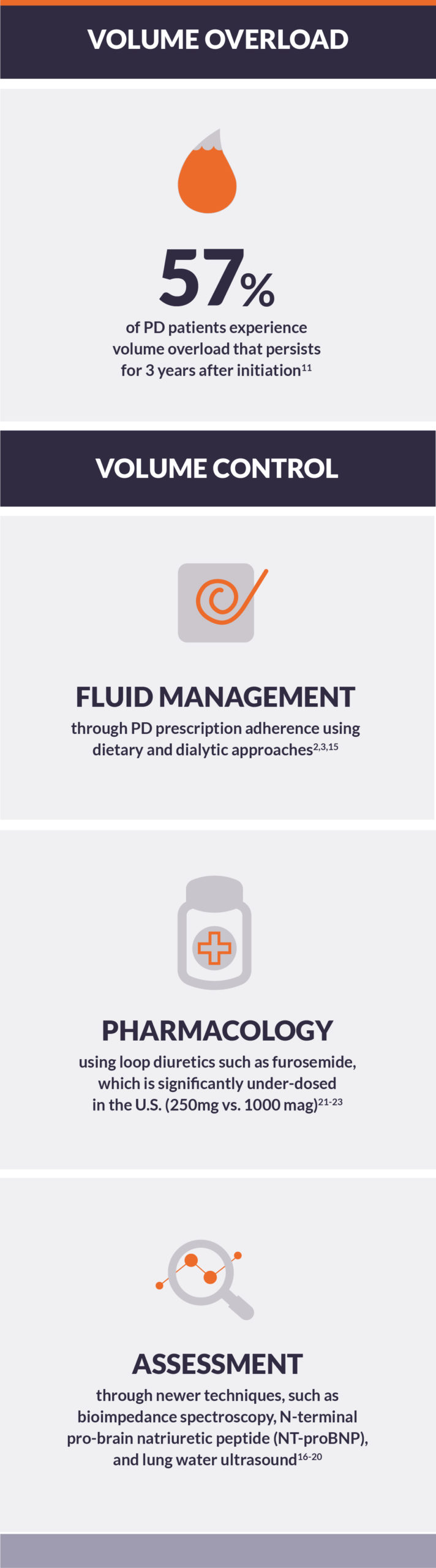
Volume overload is one of the most common complications of PD.3 Appropriate PD prescription and continuous assessment of hydration status are critically important.3 Dialytic and nutritional management of salt and water is as important as weekly clearance of urea.2
- In a prospective cohort study of more than 1,000 PD patients across Europe, the prevalence of relative volume overload was 57% at PD initiation and persisted for the duration of the 3-year study.11
- In a small, randomized clinical study comparing a volume management educational intervention to conventional care, patients in the intervention group had improved volume status and fewer volume-related hospitalizations.12
Achieving euvolemia through PD prescriptions
High-quality PD prescriptions should aim to achieve euvolemia.3 An important component of this is maximizing ultrafiltration to the end of targeting “dry” weight.13 In the U.S., dry weight assessment in PD patients is often limited to monitoring edema and blood pressure (BP) without medication.14
- Dietary approaches to managing fluid include restriction of salt and water intake, and glycemic control.2
- Dialytic approaches to managing fluid include applying results of peritoneal equilibration testing, increasing adherence to the PD prescription, adjusting dwell time and fill volume, increasing the number of exchanges during each 24-hour interval, and use of icodextrin during a long-day dwell in high transporters.1,15
- Both traditional measurements (body weight, pedal edema, and BP3) and newer assessment techniques (bioimpedance spectroscopy, N-terminal pro-brain natriuretic peptide (NT-proBNP), and lung water ultrasound) may be useful to assess volume status.16–20
- A changing trend in the ratio of extracellular water to total body water may be indicative of worsening hydration status, but the trend may also reflect worsening inflammation or hypoalbuminemia.19
Prescribing diuretics to achieve euvolemia
Pharmacologic interventions should be applied in addition to making attempts to maximize adherence to the PD prescription.21
- Loop diuretics, unlike thiazide diuretics, are a class of medications that can be effectively used in advanced chronic kidney disease and end-stage kidney disease to increase urine production.21
- Once-daily furosemide (e.g., at 250 mg per day) can be an especially useful tactic in PD patients who possess residual kidney function (RKF), but have trouble achieving euvolemia.22
- In a trial of 62 patients on continuous ambulatory PD, use of furosemide increased 24-hour urine volume by approximately 350 mL and 24-hour urinary sodium excretion by more than 3 mmol after one year.22
- In a trial of 51 patients on continuous ambulatory PD, a “triple diuretic” regimen of furosemide (1000 mg/day), hydrochlorothiazide (100 mg/day), and spironolactone (50 mg/day) increased 24-hour urine volume by over 400 mL after 6 months, relative to a regimen of furosemide (1000 mg/day) alone.23
- The “triple diuretic” regimen also improved hydration status, as measured by bioimpedance spectroscopy.23
BP control as a core parameter in assessing volume control
With a conventional definition of >140/90 mmHg, over 90% of patients initiating PD were hypertensive.24Improvements in BP control were observed up to one year after initiating PD, however, these deteriorated over time.24
- The optimal level of BP in PD patients is unknown—partly because of the absence of randomized clinical trials of BP targets in PD patients, and partly because of inconsistent findings in observational studies.25
- Some studies have suggested intuitive associations of BP and increased cardiovascular and mortality risk.25,26
- Others have reported that systolic BP below 110 mmHg is associated with increased risk of morbidity, likely as a result of confounding by cardiac function.25
Conclusion
PD is inherently customizable as a home therapy, providing many opportunities for the care team and patient to achieve volume control. However, the mechanics of PD partially depend on the transport status of the peritoneum, not an extracorporeal machine. Each patient presents unique challenges and conditions that may change due to complications and/or duration on PD, increasing the need for routine and thoughtful management of hydration status. PD on “autopilot” may result in poor outcomes in the long run, but PD with active monitoring can improve clinical outcomes.1,15