When is More Frequent Hemodialysis Beneficial?
In 2017, Medicare Administrative Contractors (MACs) began to promulgate draft local coverage determinations that include restrictive language regarding Medicare reimbursement for additional hemodialysis sessions. An important element of the draft determinations is medical justification, or the clinical conditions that constitute evidence-based rationale for the prescription of more frequent hemodialysis.
Suri and Kliger, who were both investigators in the Frequent Hemodialysis Network (FHN) trial, posed and answered this timely question in a thoughtful narrative review that appears in the July/August issue of Seminars in Dialysis. Suri and Kliger described 5 situations in which they “…believe frequent hemodialysis is likely to be most beneficial.”1
These situations are:
“FOR REDUCTION OF LEFT VENTRICULAR HYPERTROPHY, ESPECIALLY IN PATIENTS WITH MINIMAL TO NO URINE OUTPUT”
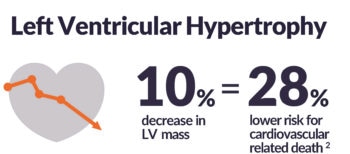
Left ventricular hypertrophy (LVH) is an adaptive response to increased cardiac work, typically caused by combined pressure and volume overload. Regression of LVH may reduce cardiovascular risk, including the incidence of heart failure, complications after myocardial infarction, and sudden arrhythmic death. 3
Diurnal and nocturnal schedules in the FHN trial reduced left ventricular mass by 14 (10%) and 11(8%) g, respectively, relative to 3 sessions per week.4,5 Comparable efficacy was observed in an earlier trial of nocturnal hemodialysis.6
“REFRACTORY VOLUME OVERLOAD AND/OR HIGH INTERDIALYTIC FLUID GAINS THAT CANNOT BE CONTROLLED ON THREE TIMES WEEKLY HEMODIALYSIS”
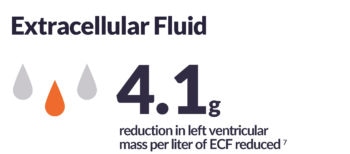
In hemodialysis patients, volume management involves two complementary tasks: managing interdialytic fluid load between treatments and managing ultrafiltration intensity during treatment. Although the latter task has garnered great attention in recent years, the former task is tremendously important. As measured by bioimpedance spectroscopy, chronic fluid overload is associated with 42% to 63% higher risk of death, relative to euvolemia.8
If volume cannot be adequately managed with diuretics (in patients with residual function) or dietary counseling regarding sodium and fluid intake, the most straightforward way to reduce the interdialytic fluid load may be to increase hemodialysis frequency:9 Raimann and colleagues showed that 6 versus 3 sessions per week reduced time-integrated fluid load by 3 liters/day in the FHN Daily Trial.7
If treatment hours are increased while treatment frequency is increased, then the ultrafiltration rate can simultaneously be reduced.10
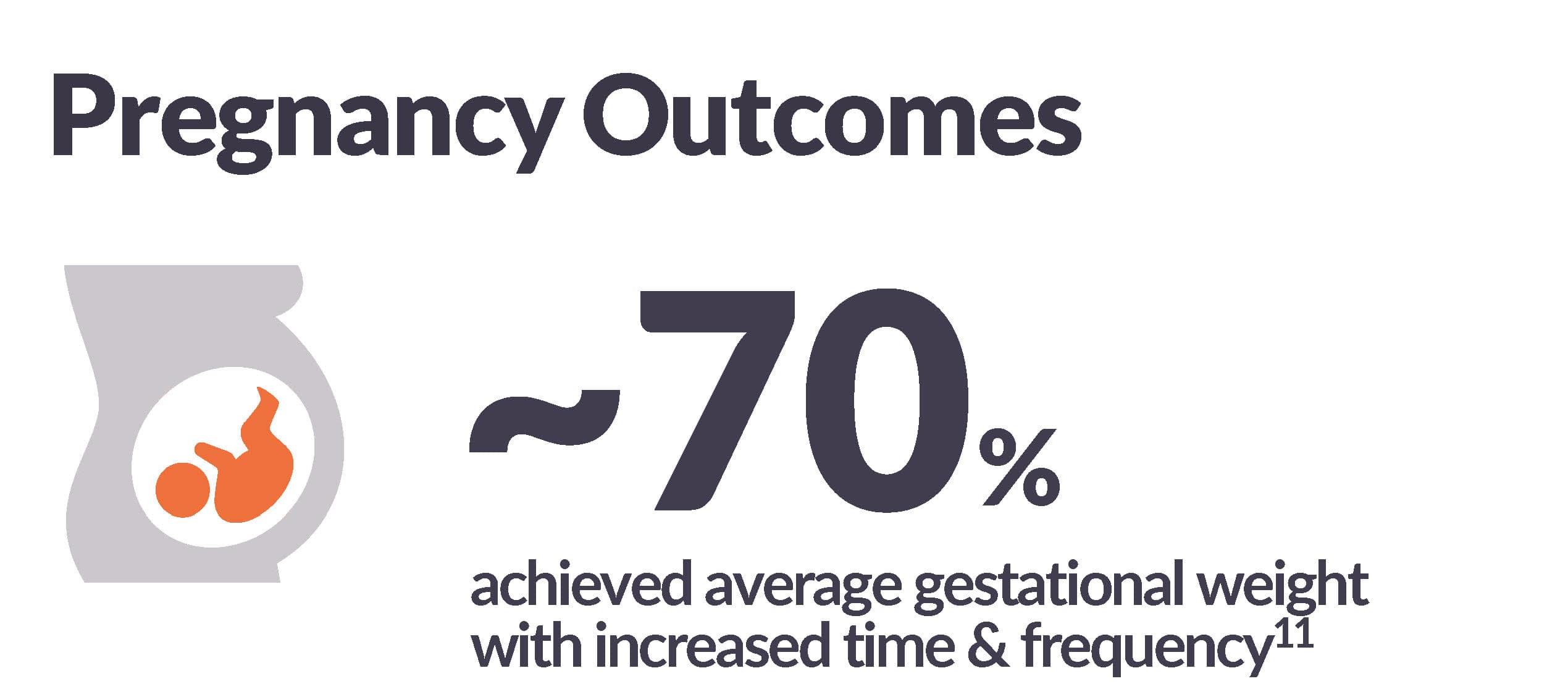
“PREGNANCY”
The Kidney Disease Outcomes Quality Initiative (KDOQI) Clinical Practice Guideline for Hemodialysis Adequacy includes the following ungraded suggestion: “During pregnancy, women with end-stage kidney disease should receive long frequent hemodialysis either in-center or at home, depending on convenience.”12

“FOR PATIENTS WANTING TO TRY FREQUENT HEMODIALYSIS FOR POTENTIAL LIFESTYLE OR QUALITY OF LIFE BENEFITS”
Health-related quality of life (HRQOL) is not only associated with clinical outcomes in dialysis patients, but also highly valued by patients. In the FHN Daily Trial, 6 versus 3 sessions per week improved both physical and mental HRQOL.4 In fact, in all randomized trials of frequent versus conventional hemodialysis, frequent therapy improved both physical and mental HRQOL, despite various degrees of statistical significance.4,5,6 Notably, frequent hemodialysis sharply reduces post-dialysis recovery time.6,13
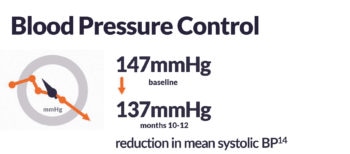
“SEVERE HYPERTENSION AND/OR SEVERE HYPERPHOSPHATEMIA THAT ARE UNCONTROLLABLE WITH THREE TIMES WEEKLY HEMODIALYSIS”
According to the most recent data from the DOPPS Practice Monitor, more than 28% of hemodialysis patients have pre-dialysis systolic blood pressure ≥160 mmHg and almost 37% of patients have 3-month mean serum phosphorus >5.5 mg/dL, despite extension application of both antihypertensive agents and phosphate binders.15 Using multiple strategies to lower blood pressure in patients on thrice-weekly hemodialysis may not lead to positive outcomes; a recently published pilot study found that patients who were randomly assigned to a lower blood pressure target range manifested higher risks of intradialytic adverse events (e.g., cramps, nausea/vomiting, and loss of consciousness), vascular access thromboses, and hospitalization.16
Frequent hemodialysis is an alternative strategy that reduces both systolic blood pressure and the need for antihypertensive agents.13 In addition, because phosphorus clearance is primarily time-dependent, frequent hemodialysis, when accompanied by more treatment hours per week, reduces serum phosphorus and the need for phosphate binders.6
Importantly, Suri and Kliger wrote that this situation “may be particularly important in patients with ongoing end-organ damage from hypertension, or calciphylaxis.”1 In other words, ongoing treatment with frequent hemodialysis may be justified, if not required.1
Conclusion
There appears to be good consensus among two teams in the nephrology community about medical justification for additional hemodialysis sessions. Multiple applications are supported by randomized clinical trials and well-designed observational cohort studies.
Potential Risks
Not everyone will experience the reported benefits of more frequent hemodialysis. All forms of hemodialysis involve some risks. When vascular access is exposed to more frequent use, infection of the site, and other access related complications may also
be potential risks.
Certain risks associated with treatments are increased when performing solo home hemodialysis; if patients experience needles coming out, blood loss, or very low blood pressure during solo home hemodialysis, they may lose consciousness or otherwise become impaired during any health emergency which, when alone, could result in significant injury or death.
Certain risks associated with hemodialysis treatment are increased when performing nocturnal therapy due to the length of treatment time and because the patient and care partner are sleeping.
