Hypertension in Dialysis Patients
The link between hypertension, left ventricular hypertrophy, heart failure, and sudden death is clear. In the dialysis population, persistent hypertension is observed in the majority of patients, making it a fundamental and unmet challenge. Accumulating evidence shows that ambulatory blood pressure is a better predictor of survival than in-unit blood pressure—and, importantly, that ambulatory blood pressure is linearly associated with risk of cardiovascular events.1,2
As clinicians, how should we respond to this challenge? A recent European consensus statement, published in the Journal of Hypertension, offers insights.3
The article outlined the diagnosis, epidemiology, pathogenesis, and treatment of hypertension in patients on dialysis. The authors emphasized the need to focus on correcting the primary mechanisms of hypertension: sodium and volume excess.
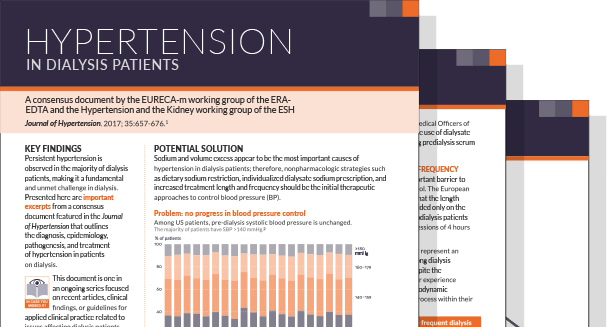
Hypertension In Dialysis Patients Recent Findings
Download PDFNon-pharmacological strategies to reduce blood pressure were suggested as initial therapeutic approaches, specifically3:
- Reduce salt intake
- Individualize dialysate sodium
- Increase treatment length and frequency
As multiple randomized clinical trials have reported, patients assigned to longer or more frequent dialysis regimens achieve better BP control, with reduced dependence on antihypertensive medications.