Standardized Kt/V on Home Hemodialysis: Does It Matter?
Hemodialysis adequacy has historically been assessed through the lens of Kt/V. Standardized Kt/V is a metric that specifically permits comparisons of urea clearance among heterogeneous hemodialysis schedules. Current clinical practice guidelines from the Kidney Disease Outcomes Quality Initiative (KDOQI) suggest a target standardized Kt/V of 2.3, and a minimal standardized Kt/V of 2.1.1 In principle, these targets are applicable to both in-center hemodialysis and home hemodialysis alike. However, there are few studies that correlate standardized Kt/V with clinical outcomes on home hemodialysis. This gap in the literature begs a surprisingly simple question: is standardized Kt/V a useful tool for evaluating home hemodialysis patients, who tend to dialyze more frequently than 3 times per week?
In the March issue of the Clinical Journal of the American Society of Nephrology, Rivara2 and colleagues analyzed the association of standardized Kt/V with an array of clinical outcomes, including biochemistry, volume-related markers, mortality, and hospitalization in both home hemodialysis and in-center hemodialysis patients. The study comprised patients who initiated maintenance dialysis between 2007 and 2011, received care for at least 60 days in a single facility operated by a large dialysis organization, and were exclusively treated with home hemodialysis or in-center hemodialysis for at least 45 days. Standardized Kt/V was characterized by the mean value during the first quarter of home hemodialysis or in-center hemodialysis, and categorized into ranges of less than 2.1, between 2.1 and 2.3, and greater than 2.3. Biochemical outcomes comprised potassium, calcium, phosphorus, and bicarbonate, and volume-related markers were weekly interdialytic weight gain and pre-dialysis systolic blood pressure. Times to death and first hospitalization were also assessed.
There were 2,373 home hemodialysis patients and over 109,000 in-center hemodialysis patients in the study cohort.
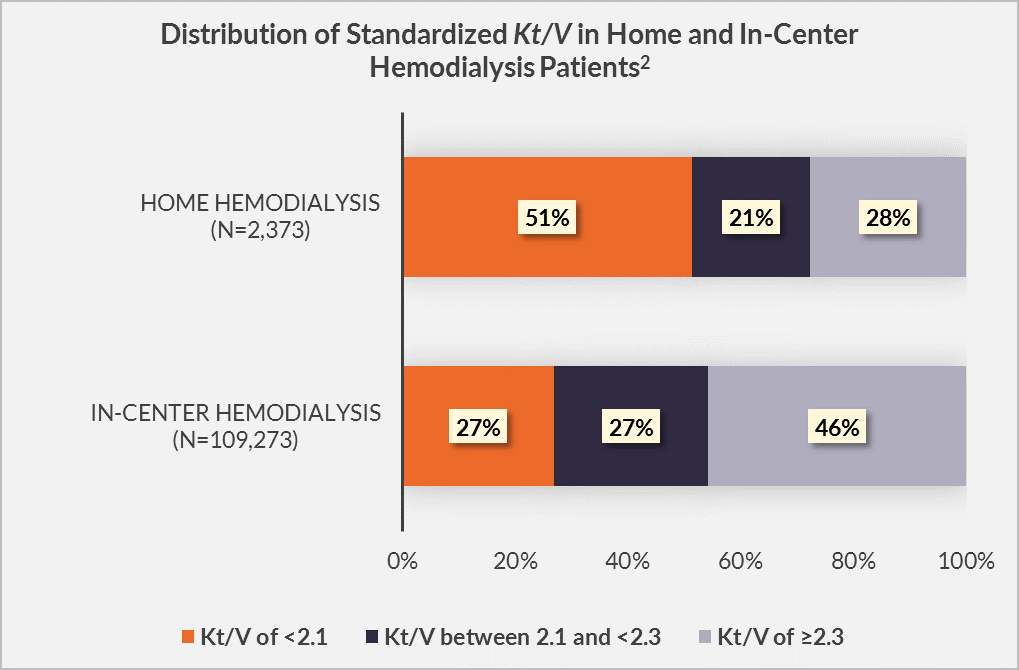
Among home hemodialysis patients, who underwent a median of 5 sessions per week, 51% had standardized Kt/V less than 2.1, 21% had standardized Kt/V between 2.1 and 2.3, and 28% had standardized Kt/V greater than 2.3.
In contrast, among in-center hemodialysis patients, who underwent a median of 3 sessions, 27% had standardized Kt/V less than 2.1, 27% had standardized Kt/V between 2.1 and 2.3, and 46% had standardized Kt/V greater than 2.3._
In both settings, female sex was much more likely in patients with standardized Kt/V greater than 2.3 than in patients with standardized Kt/V less than 2.1.
Some associations of standardized Kt/V with biochemical outcomes were statistically significant among home hemodialysis and/or in-center hemodialysis patients, but none were clinically meaningful. Interestingly, interdialytic weight gain was positively associated with standardized Kt/V in both home hemodialysis and in-center hemodialysis patients. Among home hemodialysis patients, there were no significant associations between standardized Kt/V and adjusted hazards of death, first hospitalization, and transfer to in-center hemodialysis, whereas among in-center hemodialysis patients, standardized Kt/V less than 2.1 (versus between 2.1 and 2.3) was associated with significantly higher adjusted hazards of death and first hospitalization. Of course, we should keep in mind that these associations are functions of standardized Kt/V during the first 13 weeks of home hemodialysis or in-center hemodialysis.
What can we conclude from this study? On the surface, it appears that a low standardized Kt/V in a patient on conventional in-center hemodialysis is predictive of poor clinical outcomes, but not predictive of other biochemical outcomes. On the other hand, in a patient on frequent home hemodialysis, standardized Kt/V appears to be a rather useless tool for predicting times to death, hospitalization, or discontinuation of home hemodialysis. Of course, a large majority of home hemodialysis patients in this study were prescribed frequent hemodialysis with low-volume dialysate equipment. Hemodialysis on 5 sessions per week shortens the mean duration of the gap between consecutive dialysis sessions and likely eliminates the 2-day gap that is inherent in conventional in-center hemodialysis. Increased hemodialysis frequency reduces time-integrated fluid load and blood pressure. It is conceivable that patients on frequent home hemodialysis manifest similar outcomes across a wide range of standardized Kt/V values because their cardiovascular health status is essentially homogenized. In other words, cardiovascular health status may be more important than the degree of small solute clearance.
In clinical practice, an important question stands: how should a home hemodialysis patient be evaluated each month? Is a high standardized Kt/V value a sign of success? Is a low standardized Kt/V value a cause for alarm? Based upon the data from Rivara and colleagues, the answer to the latter pair of questions is “no.” Perhaps the patient should be evaluated in alternative ways, including self-reported health status (e.g., the response to the straightforward inquiry, “How do you feel?”) and physical measurements of cardiovascular health, including blood pressure, echocardiographic measurements, and even measurements of N-terminal pro-brain natriuretic peptide (NT-proBNP). After these data are evaluated, perhaps classical biochemical outcomes and measurements of solute clearance could be considered. Ultimately, for patients on frequent home hemodialysis, starting and ending an evaluation of the efficacy of the dialysis prescription with a cursory review of standardized Kt/V appears to be incomplete.
