Recasting Kidney Failure as Cardiovascular Disease
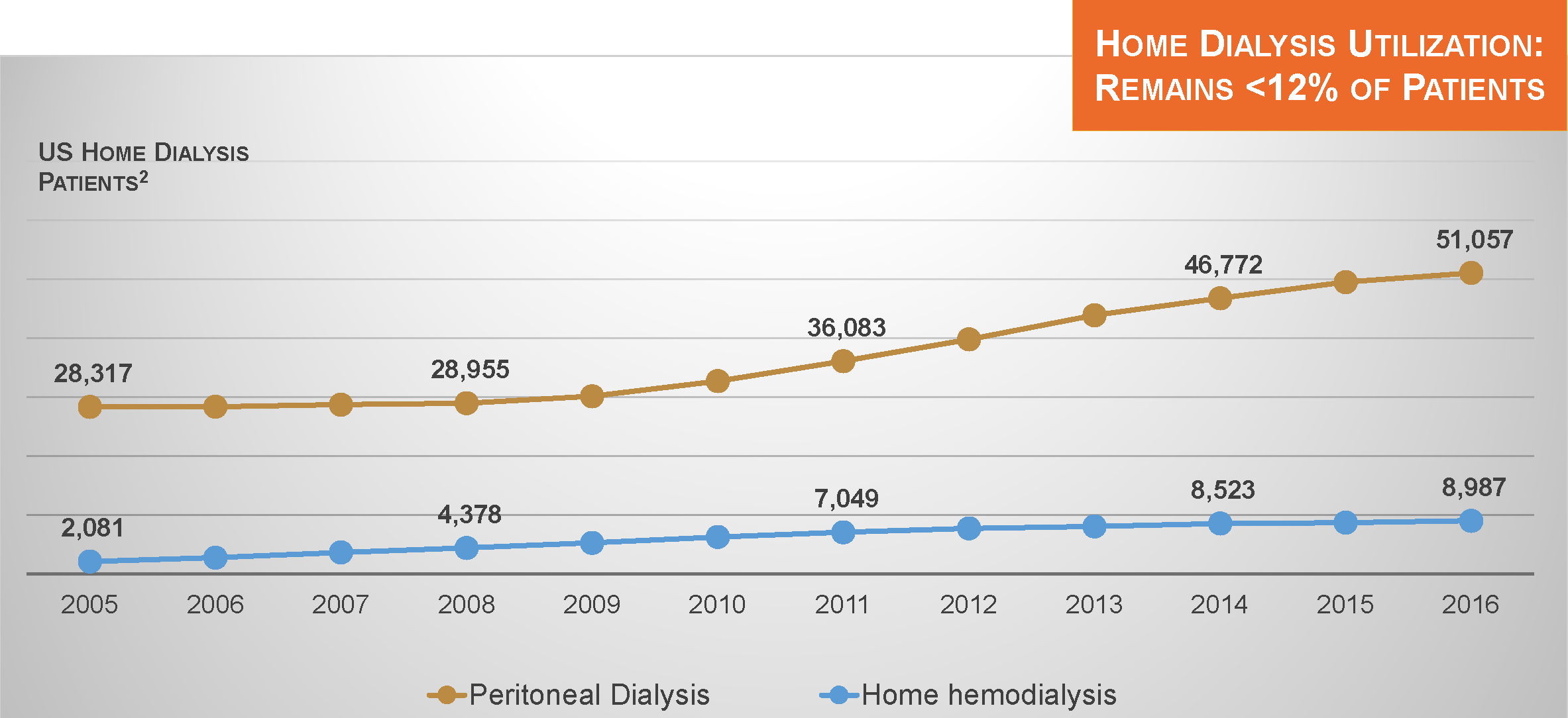
Total Medicare expenditures on the health care of patients with permanent kidney failure have steadily risen to more than $35 billion per year, although per capita expenditures on the care of dialysis patients have been relatively stable in recent years.1 This conflict in trends can be readily explained by the seemingly unstoppable increase in the number of people undergoing chronic dialysis.
Dialysis Patient Population Growth
Today, that number exceeds 510,000. Nevertheless, the annualized rate of growth in the dialysis patient population has recently slipped below 2%.
Learn MoreCardiac Arrhythmia: An Ominous Side Effect of Thrice-weekly Hemodialysis?
Many studies represent incremental gains in our understanding of human pathophysiology. Some studies, especially large randomized clinical trials, can singlehandedly change the standard of care. Other studies, at the most unexpected times, flash a signal that raises the question of whether the widely accepted standard of care is simply inadequate.
In the April 2018 issue of Kidney International, Prabir Roy-Chaudhury and colleagues published one such study. These investigators reported data from a prospective, multicenter study, the Monitoring in Dialysis (MiD) Study, which was conducted in both the United States and India and aimed to estimate the proportion of thrice-weekly hemodialysis patients who experienced clinically significant arrhythmias during 6 months of follow-up.
Learn MoreHypertension in Dialysis Patients
The link between hypertension, left ventricular hypertrophy, heart failure, and sudden death is clear. In the dialysis population, persistent hypertension is observed in the majority of patients, making it a fundamental and unmet challenge. Accumulating evidence shows that ambulatory blood pressure is a better predictor of survival than in-unit blood pressure—and, importantly, that ambulatory blood pressure is linearly associated with risk of cardiovascular events.1,2
As clinicians, how should we respond to this challenge?
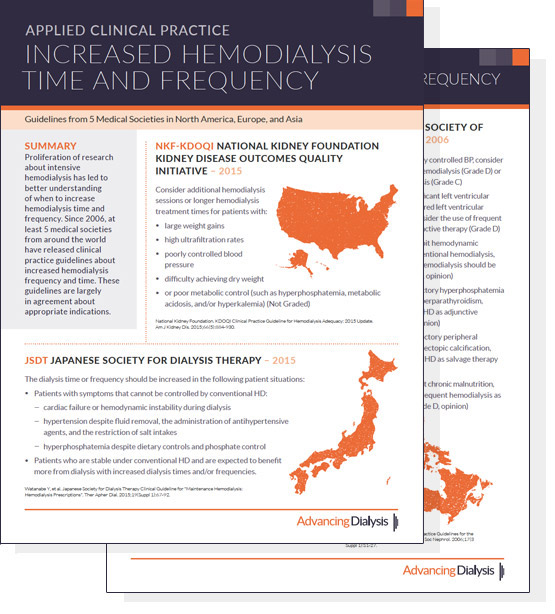
Learn MoreInternational Guidelines for Increased Hemodialysis Time and Frequency
During the past 10 years, there has been a proliferation of research about intensive hemodialysis, including both longer and more frequent hemodialysis sessions. The accumulation of data from studies has led to the development of clinical practice guidelines about hemodialysis time and frequency, with a focus on identifying indications for increasing time and frequency.
In the United States, Medicare requires medical justification for reimbursement of additional hemodialysis sessions (i.e., treatment beyond 3 sessions per week). Clinical practice guidelines not only from the United States, but also from Japan, the United Kingdom, Europe, and Canada together encourage physicians to consider applications of longer and more frequent hemodialysis sessions in patients with cardiovascular complications, including left ventricular hypertrophy and uncontrolled hypertension; hemodynamic instability during dialysis, possibly due to excessive ultrafiltration intensity; hyperphosphatemia; and malnutrition.
Learn More