Better Management of Volume with Intensive Hemodialysis
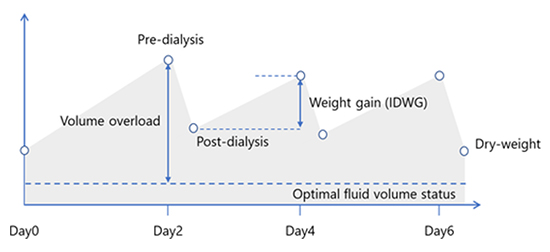
In the March issue of Nephrology News & Issues, I described the challenge of managing volume during and between hemodialysis sessions.
The root of the challenge is the intermittent nature of hemodialysis.
In the dominant schedule, intermittency is marked by 3 hemodialysis sessions per week, either on Monday-Wednesday-Friday or Tuesday-Thursday-Saturday, for 210 to 230 minutes per session.
The implication of this schedule is that we have 3 interdialytic gaps per week, including one gap of approximately 68 hours, during which fluid accumulates in the body, and we have all of 11 hours during which the hemodialysis machine removes that fluid.
Learn MoreWhen is More Frequent Hemodialysis Beneficial?
In 2017, Medicare Administrative Contractors (MACs) began to promulgate draft local coverage determinations that include restrictive language regarding Medicare reimbursement for additional hemodialysis sessions. An important element of the draft determinations is medical justification, or the clinical conditions that constitute evidence-based rationale for the prescription of more frequent hemodialysis.
Suri and Kliger, who were both investigators in the Frequent Hemodialysis Network (FHN) trial, posed and answered this timely question in a thoughtful narrative review that appears in the July/August issue of Seminars in Dialysis.
Learn MoreACE Inhibitors or ARBs: Which to Prescribe?
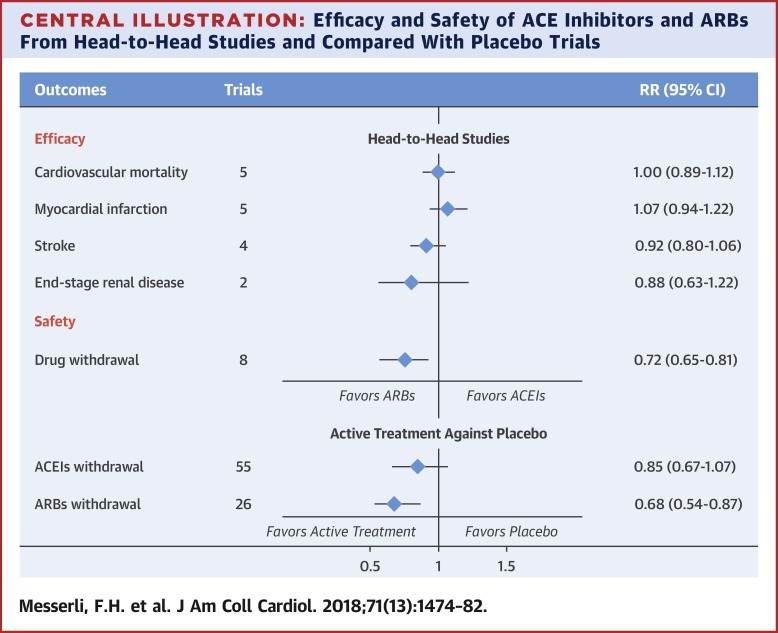
Many dialysis patients, including patients on frequent home hemodialysis, have been diagnosed with heart failure. In one large study, 31% of patients who initiated home hemodialysis already had heart failure.1 One of the cornerstones of pharmacologic therapy for heart failure is renin-angiotensin system blockade, which may be achieved with either angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs). In most clinical practice guidelines, ACE inhibitors are recommended as first-line therapy, while ARBs are recommended as a second option for patients who cannot tolerate an ACE inhibitor, typically because of a dry, persistent cough and atypically because of angioedema.
Learn MoreStandardized Kt/V on Home Hemodialysis: Does It Matter?
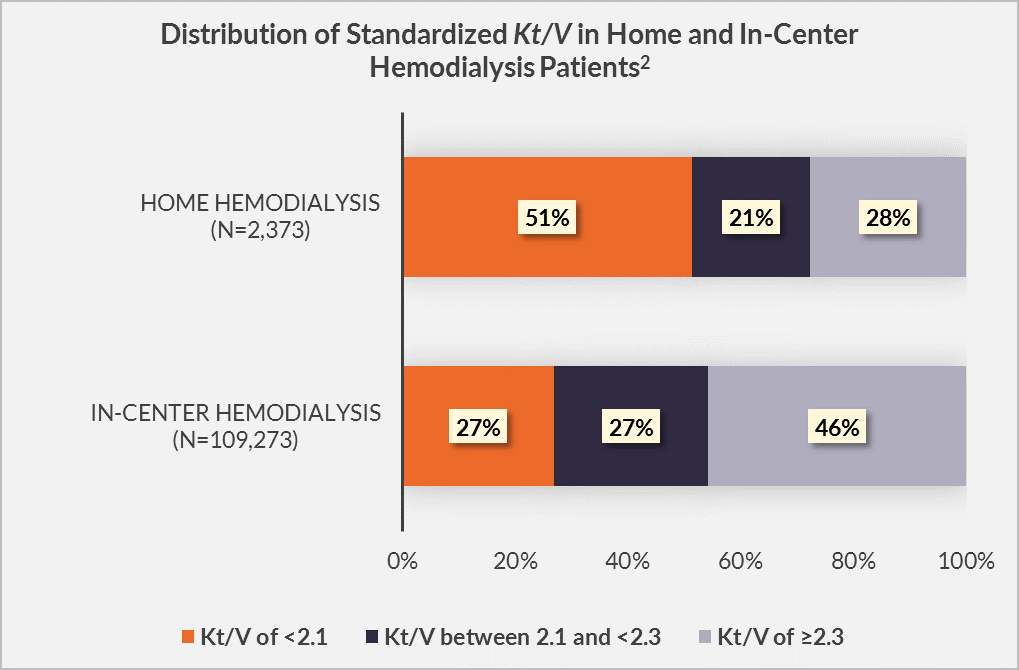
Hemodialysis adequacy has historically been assessed through the lens of Kt/V. Standardized Kt/V is a metric that specifically permits comparisons of urea clearance among heterogeneous hemodialysis schedules. Current clinical practice guidelines from the Kidney Disease Outcomes Quality Initiative (KDOQI) suggest a target standardized Kt/V of 2.3, and a minimal standardized Kt/V of 2.1.1 In principle, these targets are applicable to both in-center hemodialysis and home hemodialysis alike.
Learn More